Koita Centre for Digital Health (KCDH): Shaping the Future of Digital Health in India
Date: January 10, 2026 Location: IIT Bombay, Mumbai
The landscape of healthcare is undergoing a profound transformation, driven by the rapid integration of digital technologies. At the heart of this revolution in India stands the Koita Centre for Digital Health (KCDH) at IIT Bombay—a pioneering institution dedicated to bridging the gap between engineering, technology, and clinical practice.
A Vision for Vibrant Innovation
Established through the vision and support of Rekha and Rizwan Koita (Koita Foundation), KCDH is not just a research center; it is a vibrant department designed to make groundbreaking discoveries and train the next generation of digital health professionals.
Medical Informatics: The Bridge Between Worlds
A recurring theme during the event was the unique role of Medical Informatics. Col (Dr.) Kalyani Aadya described it simply but powerfully:
"Medical Informatics is the bridge between doctors and engineers."
In the current landscape, medical professionals and technical experts often speak "different languages." There is a fundamental language mismatch where the data scientist’s technical abstractions must be reconciled with the clinician’s grounded experience. KCDH provides the common ground where engineering expertise (Data Science, AI) meets clinical realities (Patient outcomes, diagnosis).
Doctors & Nurses: At the Frontlines of Change
Crucially, the transformation of healthcare cannot be a purely technical endeavor. Clinicians must lead innovation.
- Brilliant Ideas: Clinicians on the front lines have the most profound insights into system gaps.
- Adaptation Pressure: There is immense pressure on clinicians to adapt to digital systems. Resistance often stems from the "key-in vs. writing" friction; tools must reduce, not increase, the operational load.
- Strategic HIS Success: HIS succeeds when a core group of doctors and nurses lead the effort from the ground up, tailoring the system to specific hospital needs before heavy capital investment. Since no two hospitals function the same way—each having its own unique clinical SOPs—clinicians must lead this customization.
- Workflow Variability: As emphasized by Prof Supten Sarbadhikari, clinical workflows (including ADT—Admission, Discharge, Transfer) are not standardized globally. They vary by hospital, department, and even individual doctor, making software adaptability a critical success factor.
- The Problem of Legacy Migration: Migrating from legacy systems is a major hurdle. While starting from scratch is technically simpler, established institutions face the immense friction of data migration and system continuity.
- User Resistance Spectrum: Resistance isn't binary. KCDH identifies a spectrum of users: from those who are highly motivated but difficult to train, to those who are easy to train but difficult to motivate. A major cultural hurdle is the mismatch between motivation and training; in many institutional settings, the leader is the least motivated for digital change, creating a top-down stagnation.
- The Horse to Water Analogy: Implementation and deployment are the "easy parts"—if administration mandates it, it will happen. However, making people use the system is the real challenge. True adoption requires deep cultural change management.
- Learning, Unlearning, & Relearning: Success requires a continuous human cycle of learning, unlearning, and relearning as clinicians transition through technological generations.
- Technology Lifecycle: Digital health is not a one-time investment. Just as mobile technology advances in 1-2 year cycles, health systems must be built for continuous upgrades to remain clinically relevant and secure.
- Data Quality & Integrity: A foundational but often overlooked requirement. Standards like SNOMED CT provide the structure, but the cleaning, structuring, and integrity of data entered are paramount for operational continuity.
- The Cost of Redundancy: Redundant data entry is more than just a nuisance; it is expensive, frustrating, and a waste of time that detracts from patient care.
- Trust as a Foundation: For digital transformation to succeed, there must be a fundamental foundation of Trust. Patients and clinicians must trust that "my hospital data" is handled with the utmost integrity.
The Pillars of Transformation
The core vision is to provide the best possible healthcare to India's vast population through two broad technical pillars:
- Electronic Health Records (EHR): A system that captures the complete patient journey—from hospital entry to exit.
- Clinical Decision Support Systems (CDSS): Actively assisting clinicians with real-time data, follow-up tracking, and predictive analytics.
Breaking the "Islands of Care"
A major bottleneck is that healthcare systems often work in silos. To bridge these gaps, we must understand the Levels of Interoperability (as defined by HIMSS):
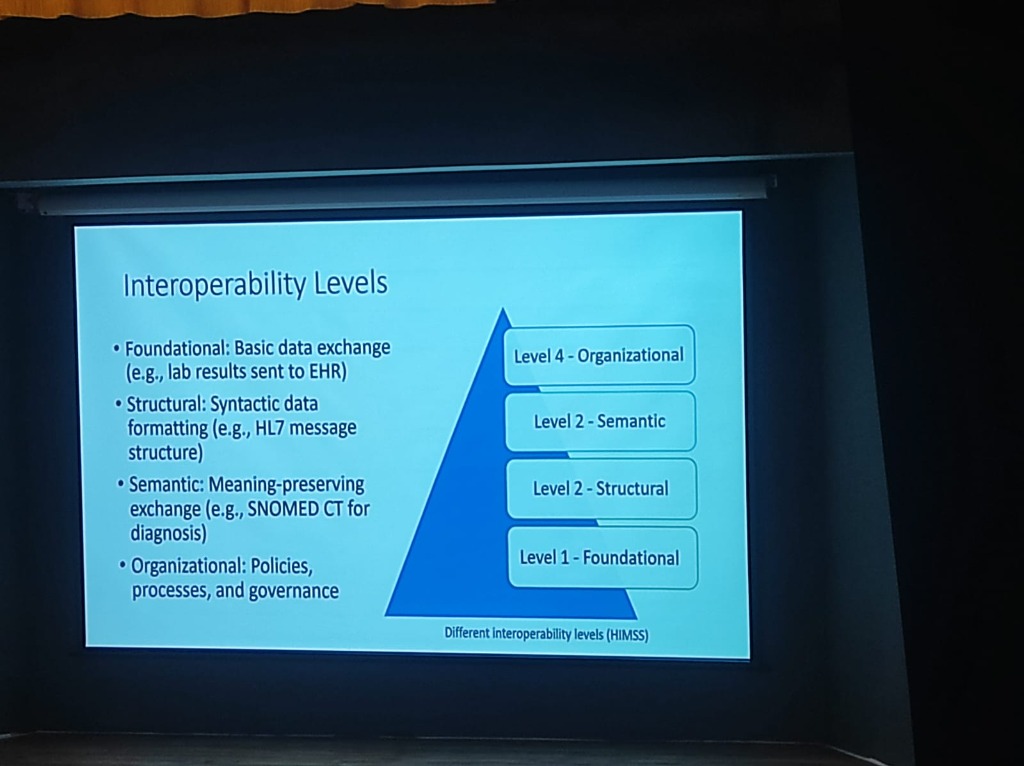
- Level 1: Foundational: Establishing basic data exchange (e.g., lab results sent to an EHR).
- Level 2: Structural: Ensuring syntactic data formatting (e.g., HL7 message structures) so data is in a readable format.
- Level 3: Semantic: Preserving meaning during exchange. Standards like SNOMED CT ensure that "CVA" in one system is understood as "Stroke" in another.
-
Level 4: Organizational: Encompassing the policies, processes, and governance that enable coordinated care across different legal and social entities.
-
The Intent Problem: Interoperability is often more of an "intent" problem than a technical one. A major cultural shift required is moving from institutional competition to a spirit of Collaboration.
The Path to Semantic Interoperability
-
The Data Journey: From Text to Trust: Bridging the gap requires a rigorous transformation of medical data:
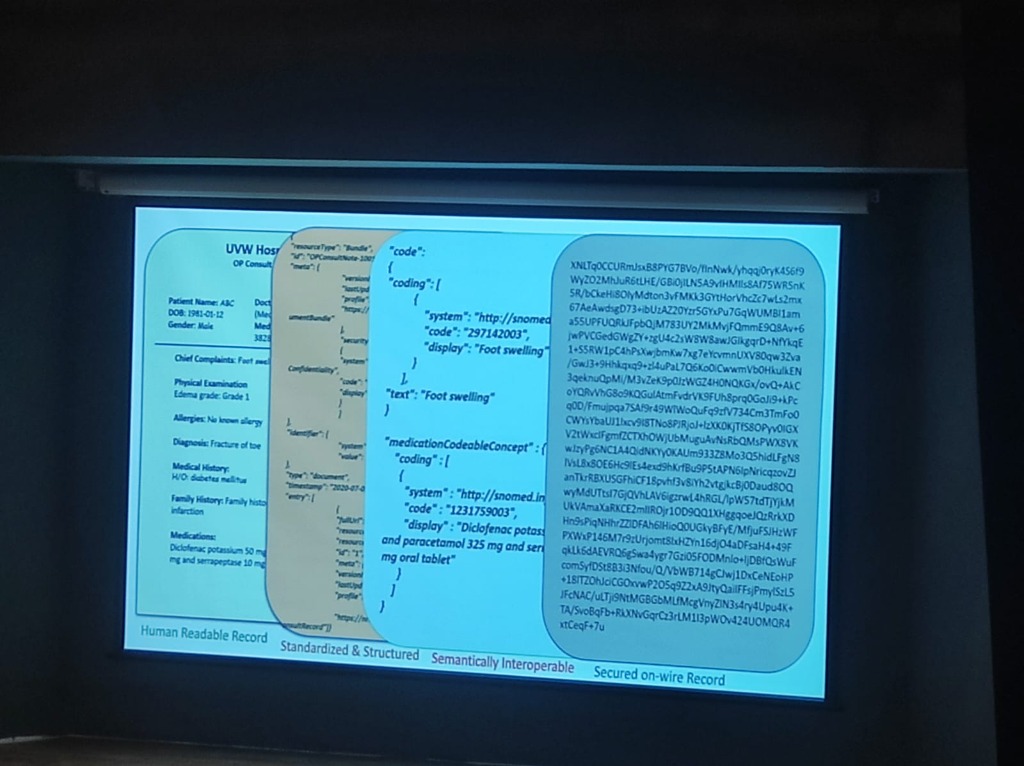
- Human Readable Record: The raw clinical input (e.g., "EDEMA grade 1", "Diclofenac Potassium 50mg").
- Standardized & Structured: Formatting the data into machine-level bundles (JSON/XML).
- Semantically Interoperable: Mapping terms to global standards like SNOMED CT (e.g., Code "297142003" for Foot swelling).
- Secured on-wire Record: Applying encryption to ensure data is protected as it moves across the network.
-
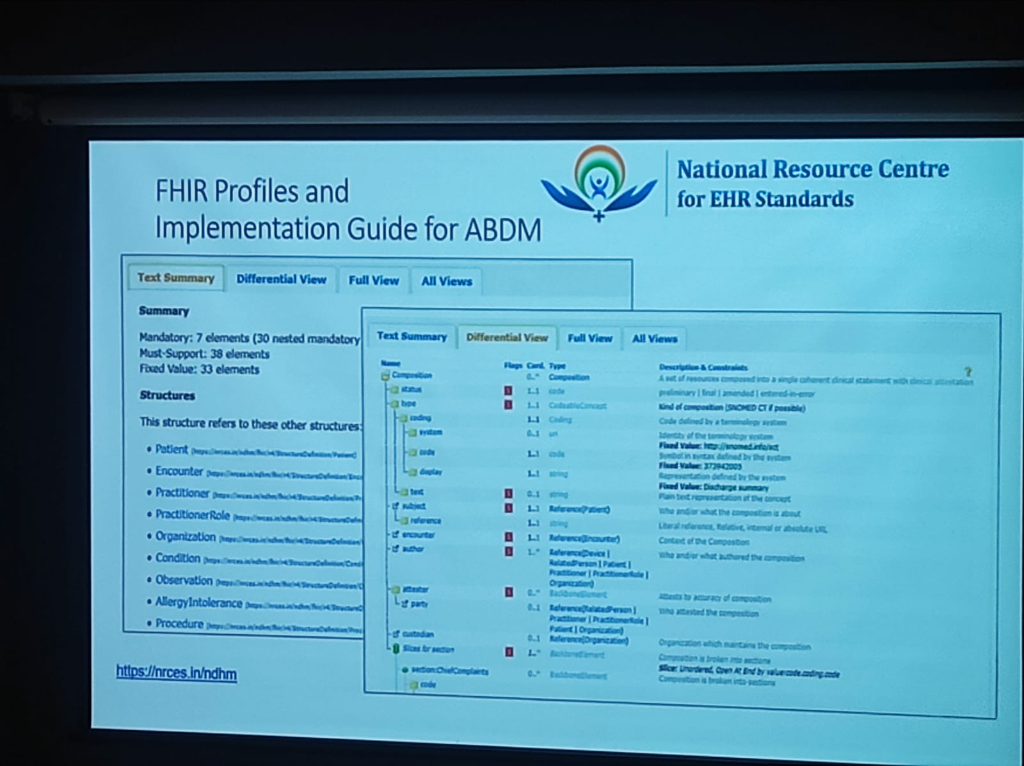
FHIR: The Blueprint for Exchange: FHIR (Fast Healthcare Interoperability Resources) is the global standard developed by HL7 International that enables this exchange. Crucially, the Ayushman Bharat Digital Mission (ABDM) uses FHIR as its primary data structure for creating India's unified health infrastructure.
-
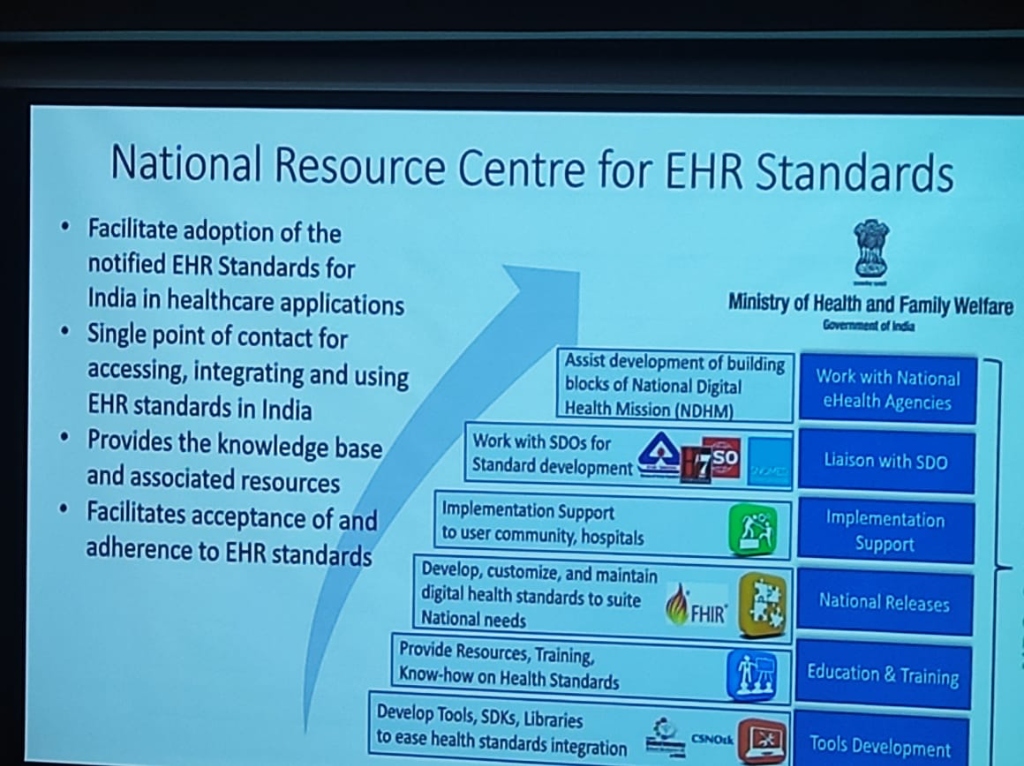
NRCeS Stewardship: As detailed by Dr. Manisha Mantri (CDAC), the National Resource Centre for EHR Standards (NRCeS) maintains the FHIR Profiles and Implementation Guides tailored for ABDM.
- Comprehensive Specs: Combining a data dictionary, discrete objects/structures, and value tables for terminology.
- Modular Resources: Providing over 145 standard structures covering Healthcare Entities (Patient, Practitioner), Clinical Information (Condition, Procedure), and Financial Information (Claims, Invoice).
-
Reusable & Extensible: FHIR is designed to be customized for specific use cases through extensible Profiles.
-
DICOM: Decoding Medical Imaging: While FHIR handles the clinical and administrative data, DICOM (Digital Imaging and Communications in Medicine) is the global specification for exchanging medical images.
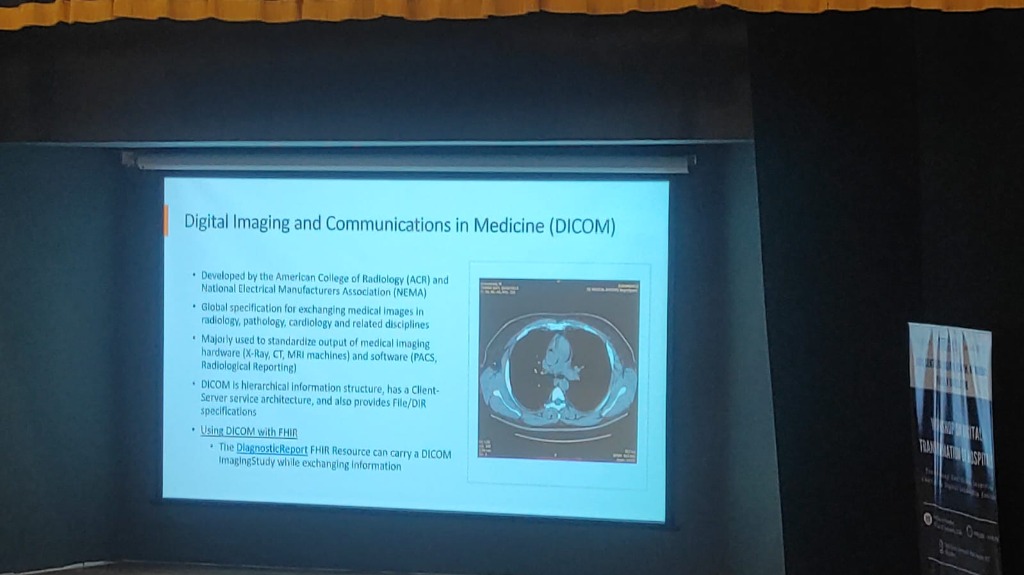
- Unified Imaging: Standardizing output from hardware like X-Ray, CT, and MRI machines to ensure seamless communication with PACS (Picture Archiving and Communication Systems).
- Clinical Inference through Metadata: Capturing critical attributes like laterality (left vs. right) and modality (CT vs. MRI), which are foundational for building advanced clinical inference models.
- DICOM & FHIR Synergy: The two standards work in tandem; for example, a FHIR DiagnosticReport resource can reference a DICOM ImagingStudy while exchanging information.
-
SNOMED CT: The Clinical Vocabulary: While DICOM captures the pixels and FHIR captures the structure, SNOMED CT provides the meaning.
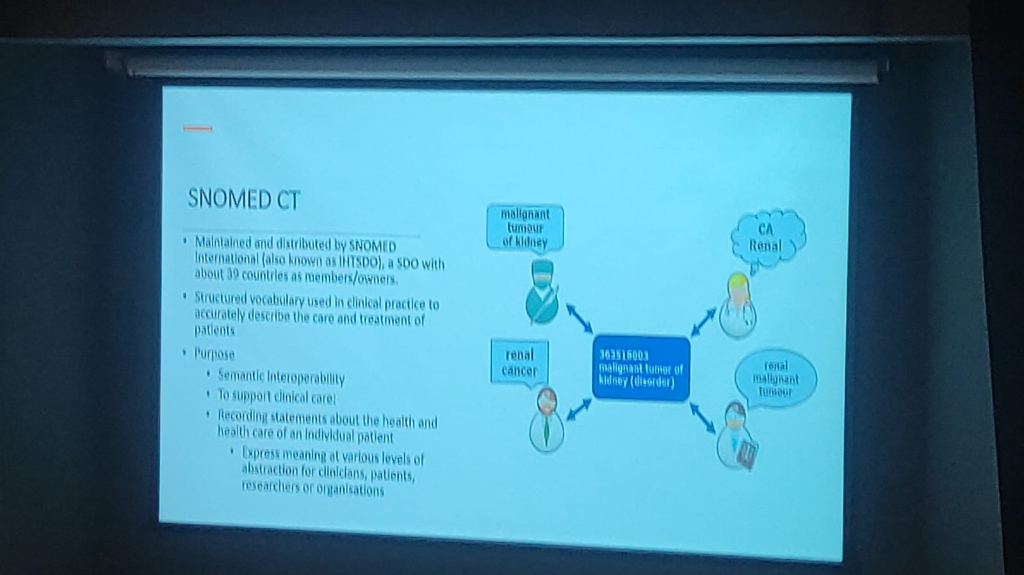
- Unified Meaning: Providing a structured vocabulary that accurately describes clinical care—for example, resolving terms like "Renal Cancer" and "Malignant tumor of kidney" to a single code (363516003).
- Automated Semantic Mapping: Enabling SNOMED CT and ICD to be mapped automatically, allowing clinicians to document with clinical precision while administrative requirements are handled in the background.
- Semantic Interoperability: Ensuring that data remains consistent and understandable across different systems, clinicians, and researchers.
- Multidimensional Abstraction: Expressing clinical meaning at various levels to support both precise detail and high-level population health analysis.
-
Advanced Analytics through the SNOMED CT Data Model: Beyond simple terminology, SNOMED CT provides a robust Data Model that simplifies complex clinical analytics.

- Relationship Mapping: The model enables associated disease analysis by linking concepts through specific attributes like Associated Morphology (e.g., Infarct) and Finding Site (e.g., Myocardium structure).
- Automated Inference: By structuring clinical data into logical hierarchies (e.g., Myocardial infarction → Necrosis of anatomical site → Myocardial necrosis), it allows for automated inference and more accurate epidemiological research.
- Data Consistency: This machine-level data model ensures that data points from diverse sources can be aggregated and analyzed without manual normalization, making large-scale clinical trials and public health surveillance far more efficient.
The "Standard Trinity": A Unified Foundation
The true power of digital health is realized when DICOM, FHIR, and SNOMED CT are integrated: - Imaging (DICOM) provides the visual evidence. - Exchange (FHIR) provides the structural pipe. - Vocabulary (SNOMED CT) provides the semantic clarity. Together, they ensure that a patient's health record is not just digital, but semantically rich, longitudinal, and universally understandable.
-
LOINC: Standardizing Lab Observations: While SNOMED CT handles clinical findings, LOINC (Logical Observation Identifiers Names and Codes) is the universal standard for identifying medical and laboratory observations.
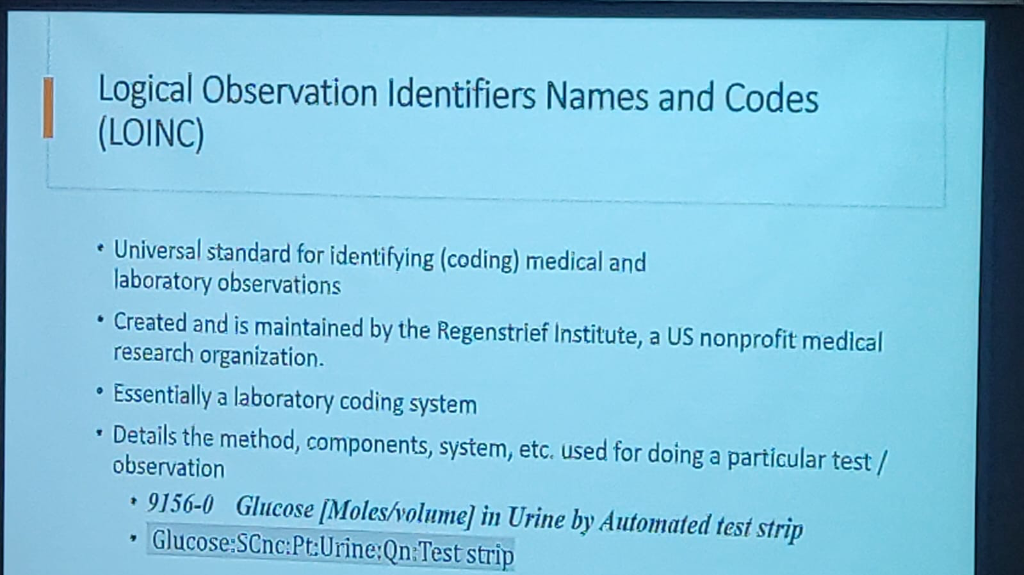
- Laboratory Precision: It details the exact method, components, and systems used for a particular test (e.g., Code 9156-0 for Glucose in Urine by automated test strip).
- Universal Coding: LOINC ensures that a "Glucose" test from one lab is understood identically by any other system, regardless of the local equipment used.
-
ICD: Disease Classification & Reporting: Maintained by the World Health Organization (WHO), ICD (International Classification of Diseases) is the global standard for health data, clinical documentation, and aggregation.

- Public Health Mandate: ICD codes are mandated for monitoring the incidence and prevalence of communicable diseases and for accurate mortality reporting.
- Epidemiological Insights: It allows government bodies to conduct epidemiological research on health trends and compare data across different periods and locations.
-
Common Identifiers (ABHA): National standards like ABHA serve as the common thread, bridging fragmented hospital numbers (MRNs) to ensure patient records are longitudinal and accurate.
- The SOP Gap: Digitization must focus on SOPs (Standard Operating Procedures), which are currently lacking across the board.
- The Build vs. Buy Dilemma: A core strategic question for any institution is whether to build from scratch (custom design and development), buy COTS (Commercial Off-The-Shelf) applications, or adopt a hybrid approach of buying and customizing.
- Phased Implementation: To minimize "teething problems," adoption must be phased and well-planned rather than a "big bang" rollout.
The Capacity Building Framework
To overcome the "Fixed Mindset" barrier, KCDH emphasizes a holistic approach to Capacity Building that fosters Cultural Agility:
- Consent-Driven Architectures: Aligning with the ABDM framework, data sharing must be built on Consent-Driven Architectures that ensure Ethical Data Sharing and patient agency.
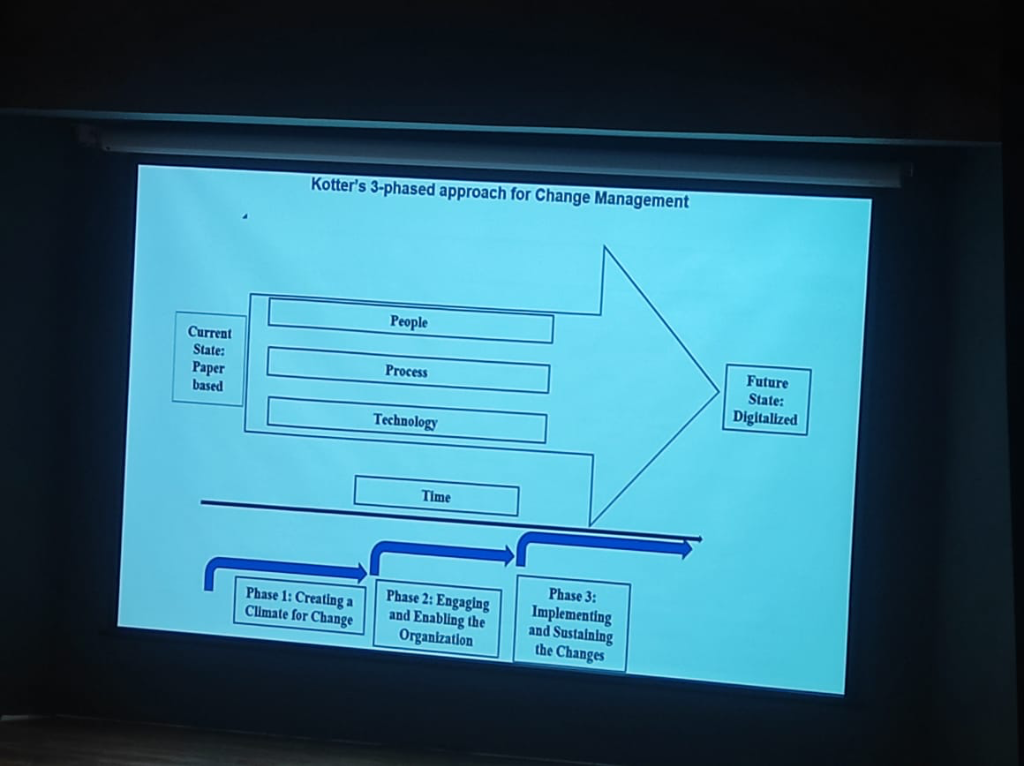
- Change Management (Kotter's 3-Phased Approach): Real transformation follows a structured journey of creating a climate for change, engaging the organization (through Champions), and finally sustaining the gains.
- Tailored Modules: Customizing digital tools for doctors and paramedical staff to ensure they serve clinical reality rather than a generic vendor vision.
- Clinician control: Physicians can audit all automated processes, ensuring that AI remains a "Decision Support" tool rather than a replacement for clinical judgment.
Digital Health at Scale: The NHA Perspective
A critical highlight from Himanshu Goel (NHA) involves the deployment of digital health solutions across India's diverse landscape. Contrary to common myths about rural digital literacy, India is demonstrating that digital health can be adopted at a staggering scale.
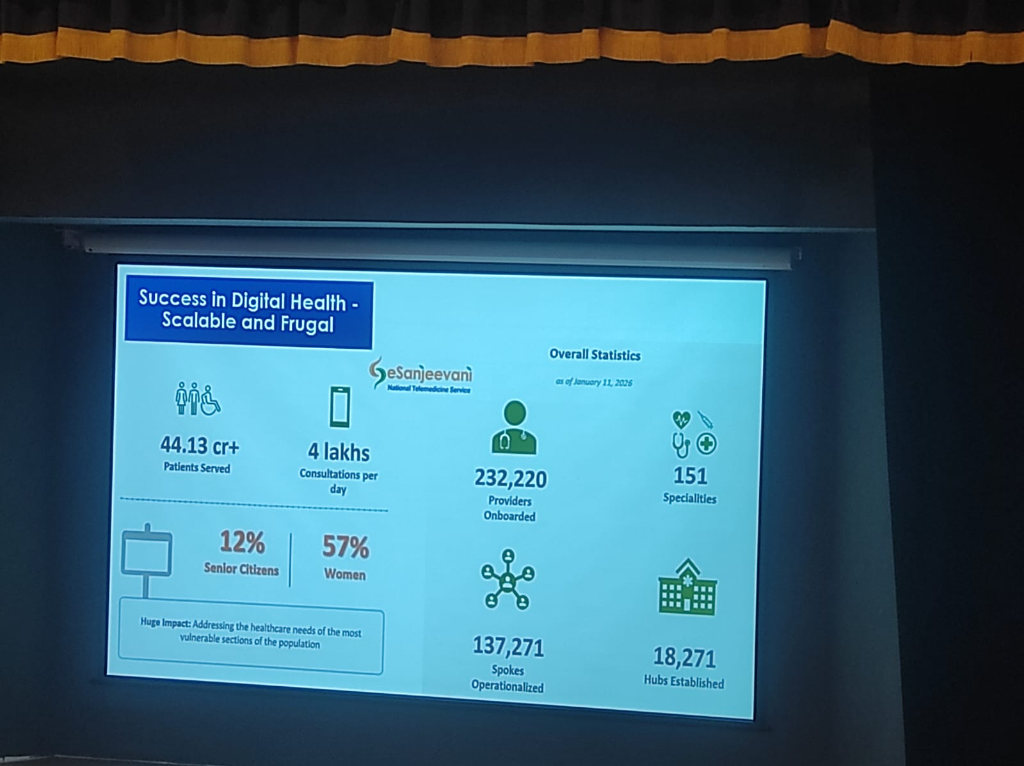 Figure: The scale of E-Sanjeevani as of January 11, 2026.
Figure: The scale of E-Sanjeevani as of January 11, 2026.
- E-Sanjeevani: Telemedicine for the Millions: Launched in 2018, the E-Sanjeevani platform has transformed healthcare access in rural areas.
- Total Patients Served: Over 44.13 Crore (441 Million).
- Daily Velocity: Currently averaging 4 Lakh (400,000) consultations per day.
- Provider Network: 232,220 providers onboarded across 151 specialities.
- Infrastructure Footprint:
- Hubs Established: 18,271 specialist hubs.
- Spokes Operationalized: 137,271 peripheral units.
- Inclusivity & Demographics: The platform is successfully addressing the needs of underserved populations:
- Women: Account for 57% of the total beneficiaries.
- Senior Citizens: Represent 12% of the user base.
- Rural Empowerment: These numbers illustrate that the rural population—connected through sub-health centers to specialists in district hospitals—is actively and effectively utilizing digital health solutions.
- The Economic Impact: Telemedicine is not just a clinical tool; it is an economic stabilizer for the rural poor.
- Time Savings: Patients save an average of 18 hours of time per consultation by avoiding travel and long hospital wait times.
- Wage Protection: For a daily wage laborer, a trip to a specialist in a city often consumes a full day. Accessing care via E-Sanjeevani saves one full day of daily wages, ensuring that seeking health doesn't lead to financial instability.
- CoWIN: Digital Orchestration at Staggering Scale:
- Beyond telemedicine, the CoWIN platform stands as a global benchmark for digital health operations.
- At its peak, the system facilitated more vaccinations in a single day than the entire populations of many countries combined. This massive orchestration proved that India's digital public infrastructure can handle load and complexity at a level previously thought impossible across such a vast geography.
India's Digital Foundation: The Internet Journey
The success of these platforms is underpinned by the massive expansion of digital connectivity across the subcontinent.
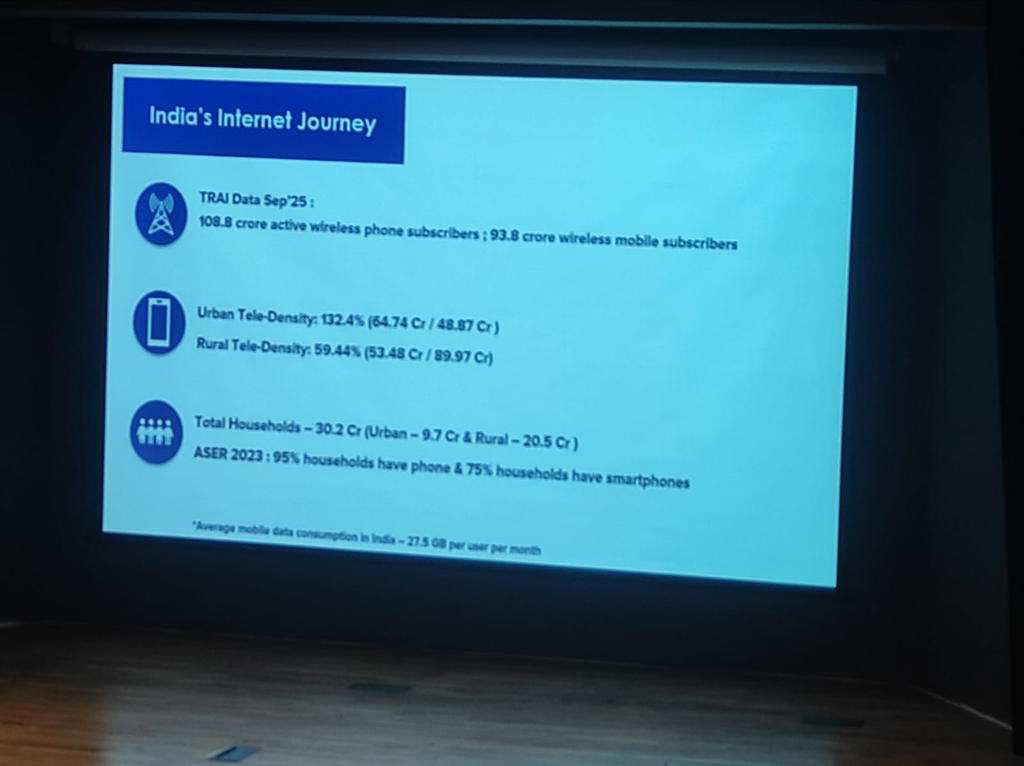 Figure: The growth of mobile and data penetration in India (Source: TRAI/ASER).
Figure: The growth of mobile and data penetration in India (Source: TRAI/ASER).
- The Connectivity Boom: As of September 2025, India has 108.8 Crore active wireless phone subscribers, with 93.8 Crore being mobile data users.
- Rural vs. Urban Tele-Density:
- Urban: 132.4% tele-density.
- Rural: 59.44% tele-density, indicating a significant yet growing footprint in the most remote areas.
- Household Penetration: 95% of the 30.2 Crore households in India have a phone, and 75% already have a smartphone.
-
Data Dominance: India remains a global leader in data consumption, with an average of 27.5 GB per user per month.
-
Champions in Rural Areas: Overcoming digital literacy and infrastructure challenges in rural regions requires identifying and empowering local Digital Champions. These peer-led advocates bridge the gap, proving that digital tools—when designed for high-friction, low-resource settings—can be mastered through Modular, hands-on training rather than academic theory.
- Standards & Infrastructure: Adopting global standards and addressing the maintenance and continuity gap in government hospital hardware to support clinical reliability.
Institutional Standards: NABH & The Maturity Path
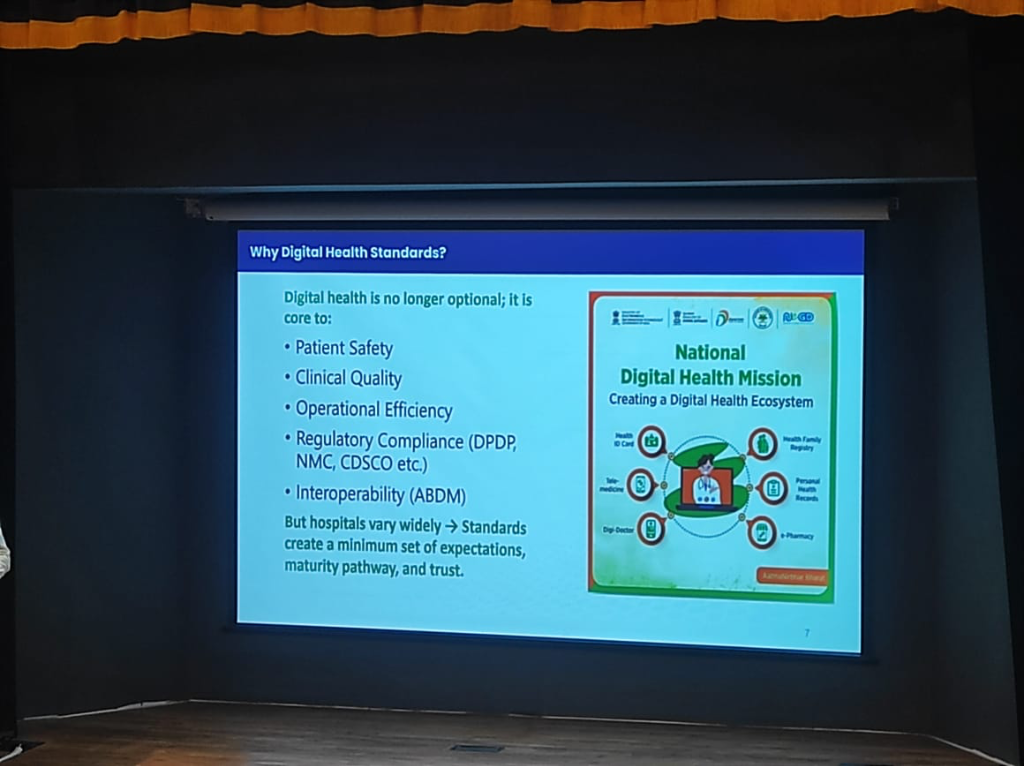 Figure: The National Digital Health Mission ecosystem, creating a unified pathway for patient safety and interoperability.
Figure: The National Digital Health Mission ecosystem, creating a unified pathway for patient safety and interoperability.
JCI vs. NABH: A Global-Local Bridge
A common question arises regarding the choice between international and national standards. While JCI (Joint Commission International) is a prestigious global benchmark, it is primarily designed for western, developed contexts where patient quality awareness and secondary infrastructure are already at a high baseline.
- The India Reality: India requires a Tiered Approach. NABH standards are explicitly designed to account for varying institutional strength, digital maturity, and geographic location (Tier 1 vs. Tier 2/3).
- Progressive Maturity: Instead of a "pass-fail" global hurdle, NABH allows hospitals to grow through tiered accreditation, making quality excellence achievable for everyone from a rural 30-bed hospital to a metropolitan multi-specialty center.
The 8-Chapter Modular Framework
To ensure structured and progressive growth, the NABH digital standards are organized into eight key chapters, covering both clinical and operational excellence:
- AAC (Access, Assessment, and Continuity of Care): Streamlining Admission, Discharge, and Transfer (ADT) and ensuring long-term care continuity.
- COP (Care of Patients): The clinical heart of the framework, digitizing core care pathways and real-time patient monitoring.
- MOM (Management of Medication): Standardizing the entire medication lifecycle, from pharmacy inventory to safe bedside administration.
- HRM (Human Resource Management): Managing the clinical and administrative workforce in a structured, digitized environment.
- IMS (Information Management Systems): Breaking down data silos to ensure True Portability of health records across the institution.
- Finance & Procurement (P&L): Transparent tracking of clinical consumables and financial throughput.
- Digital Infrastructure & Security: Foundational standards for hardware maintenance and data protection.
Breaking the Silos: A Unified Mission
As Avinash Pandey highlights, one of the greatest contributions of NABH digital standards is their ability to break organizational silos.
- The Trinity of Adoption: Successful EMR adoption is no longer just an "IT project." It is a unified mission where the Clinical, Quality, and IT teams come together.
- Standardized Quality: Quality teams provide the data integrity benchmarks, clinical teams provide the operational reality, and IT teams provide the technical backbone. This cross-functional collaboration is the key to moving from fragmented data to a cohesive digital health ecosystem.
Small-Hospital Scalability: Design for India's Reality
A common misconception is that digital standards are only for large corporate hospitals. On the contrary, NABH standards are explicitly designed to be inclusive of 30-50 bed hospitals, which form the backbone of Indian healthcare.
- Remote Adoption: Small hospitals in remote regions—from Manipur to Jammu & Kashmir—are already adopting these standards, proving that digital maturity is a function of leadership more than bed count.
Lightweight EMR Strategies: Pragmatic Digital Adoption
One of the most significant insights from the current national rollout is that Small and Medium healthcare facilities need not have a full-fledged, complex EMR to participate in the digital ecosystem. - Micro-EMR Solutions: The NHA is actively collaborating with and promoting lightweight platforms like eSushrut and eKa Care. These solutions provide the core digital building blocks (ABHA linkage, consultation logging, and report sharing) without the overhead and cost of a Tier-1 enterprise system. - Modular Growth: This strategy allows smaller clinics and nursing homes to achieve basic digital compliance almost immediately, with the path to add more complex clinical modules as they scale or their needs evolve. - Democratizing Quality: By lowering the entry barrier, even a small community hospital can achieve the same data integrity and patient safety benchmarks as a Tier-1 institution.
The ROI of Standards: Measurable Impact
Standards are not just about compliance; they are a direct driver of institutional revenue and operational velocity. Reported improvements from hospitals adopting national digital health standards include:
- Revenue Velocity & Throughput:
- 30% Average Reduction in Patient Waiting Time: Dramatically increasing patient volume and clinic efficiency.
- 20% Reduction in Discharge TAT: Faster bed turnover, allowing for more revenue-generating admissions in the same fixed facility.
- Revenue Capture & Operational Savings:
- 18% Reduction in Prescription Bounces: Direct revenue growth for hospital pharmacies by ensuring internally generated prescriptions are captured at the point of care.
- 39% Diagnostic & 15% Blood Component TAT Reduction: Faster clinical decision-making, reducing uncompensated "stagnation" time.
- Risk & Clinical Excellence:
- 10% Medication Accuracy Improvement: A critical shield against clinical errors, litigation, and adverse patient incidents.
- 100% Patient Record Access: Realizing the longitudinal health record, reducing redundant testing and improving diagnostic precision.
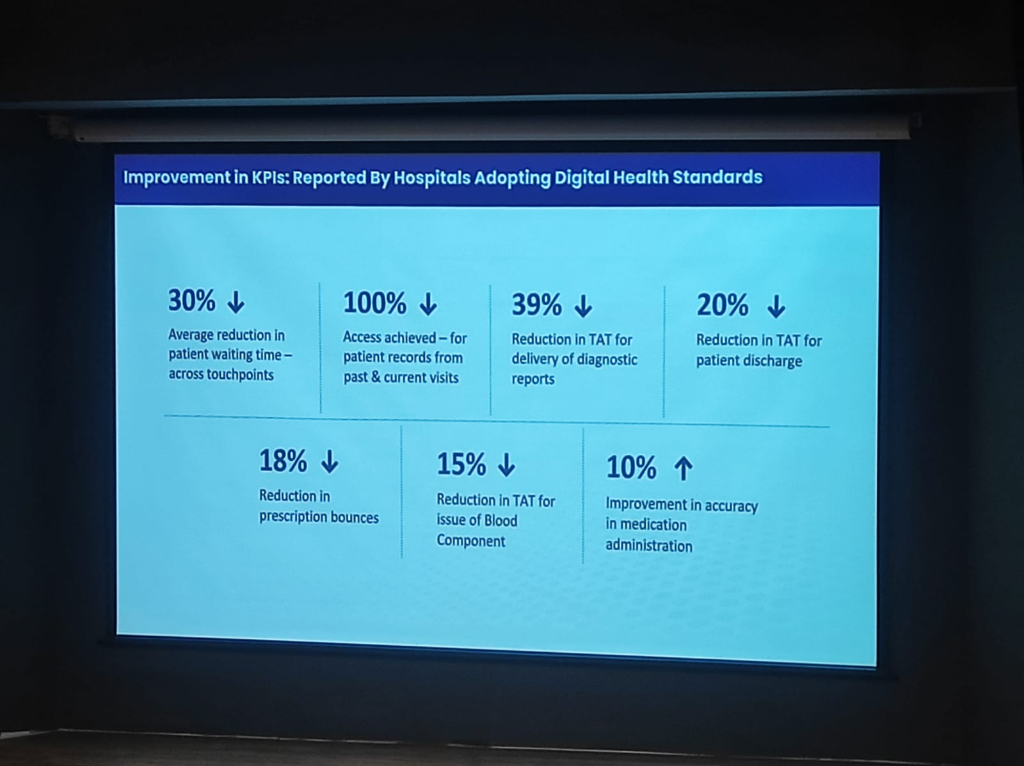 Figure: Measurable KPI improvements reported by hospitals adopting national digital health standards.
Figure: Measurable KPI improvements reported by hospitals adopting national digital health standards.
The Certification Shortcut vs. The Impact Gap
For hospitals looking to accelerate their accreditation, NABH has simplified the compliance burden. Institutions that adopt NABH-certified HIS, EMR, or Practice Management Systems (PMS) are automatically considered compliant with the digital standards. This ensures that even smaller clinics can achieve standardized quality without needing a massive internal IT department.
However, a critical distinction exists between Certification and Operational Impact:
- The M1/M2/M3 Gap: While many systems are certified for Milestones (M1/M2/M3), the actual implementation often falls into the "Photo-Upload" Trap. Instead of capturing structured, clinical-grade data, some implementers simply upload photos of paper records to meet compliance.
- Structured Data for AI: This shortcut renders the data useless for AI-driven clinical decision support. True impact requires native structured data entry at the point of care, moving beyond simple digitization of paper.
Financial & Resource Support: Bridging the Digital Divide
Achieving digital maturity represents a significant capital and operational investment, especially for smaller institutions.
- The Funding Hurdle: Small hospitals (30-50 beds) require dedicated support for Hardware Procurement, reliable connectivity, and specialized Manpower for data entry and system maintenance.
- Government Assistance: There is an urgent need for financial subsidies or grant frameworks from the government/NHA to offset these initial costs, ensuring that digital health doesn't become a "Tier-1 only" privilege.
Health Data Retention & Private Sector Friction
The path to universal adoption is paved with both policy mandates and legal complexities.
- Health Data Retention Policy: The NHA has launched a comprehensive Health Data Retention Policy. Any HMIS or health facility integrating with the national backbone must adhere to these standardized retention timelines, ensuring that longitudinal records are not prematurely archived.
- The Lobby Constraint: Despite the government's push, private sector participation remains significantly lower. In some states, attempts to mandate ABDM were met with strong opposition from medical lobbies, resulting in court stay orders that have temporarily halted aggressive implementation. The strategy has thus shifted from "force" to "facilitation and awareness."
AI Governance: Standard Adoption First
As hospitals look toward the future, the role of AI Governance and Ethical Usage becomes paramount.
- A Prerequisite, Not an Afterthought: Standards are an integral part of AI. While NABH and other bodies are yet to adopt specific AI-only standards, the adoption of data standards is the most critical prerequisite for ethical AI deployment.
- The AI Regulatory Choice: NABH has made a deliberate strategic decision to steer clear of AI standards in the current national framework. The priority is to ensure foundational data integrity, human accountability, and patient safety first, before mandating AI-specific regulatory norms.
- Fragmented Data Barrier: Fragmented, non-standardized data hinders the true potential of AI. Universal adherence to NABH digital standards is the key to unlocking clinical quality at scale.
NRCeS: Facilitating National Adoption
The success of digital health depends on a single point of contact for standards and implementation support.
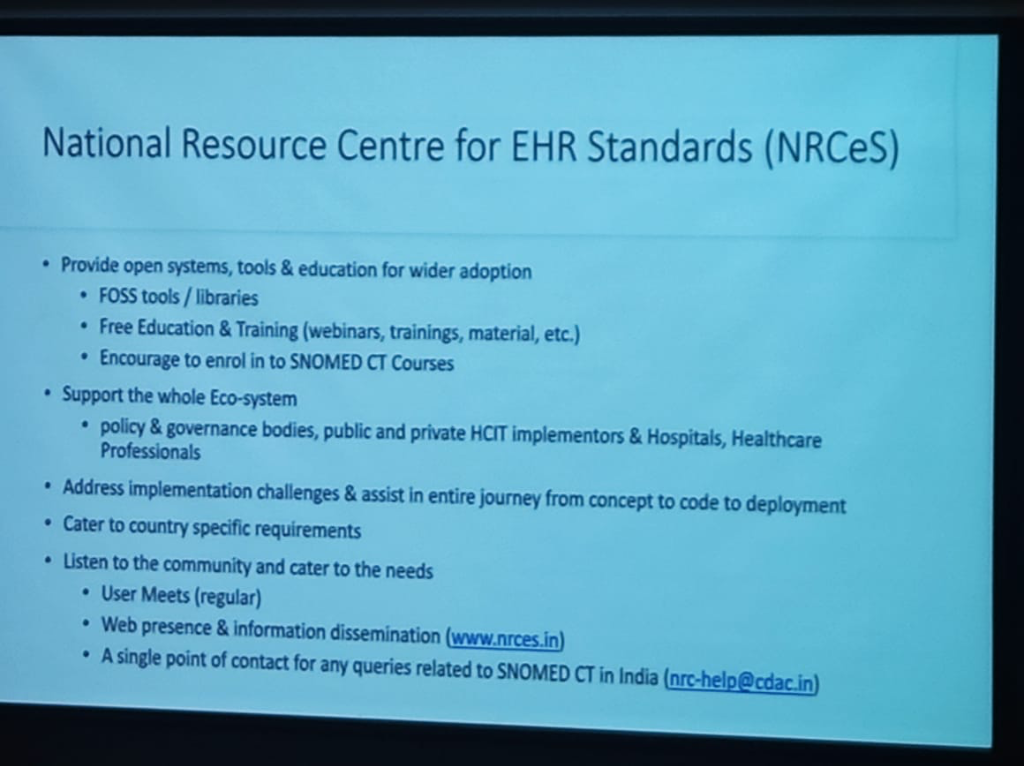
- Standards Development & Stewardship: NRCeS facilitates the adoption of notified EHR standards for India and acts as a knowledge base for associated resources.
- Co-Development & Implementation: They assist in the development of building blocks for national health missions (NDHM/ABDM) and provide hands-on implementation support to hospitals and clinicians.
- The "UPI of Healthcare": Just as UPI revolutionized finance, ABDM serves as the unified national backbone for health data exchange.
Design Thinking: Innovation for India (Dr. Richa Singh)
Following Dr. Prabhu's strategic session on entrepreneurship, Dr. Richa Singh presented a foundational framework for healthcare product development in the Indian context, centered on Design Thinking and First Principles.
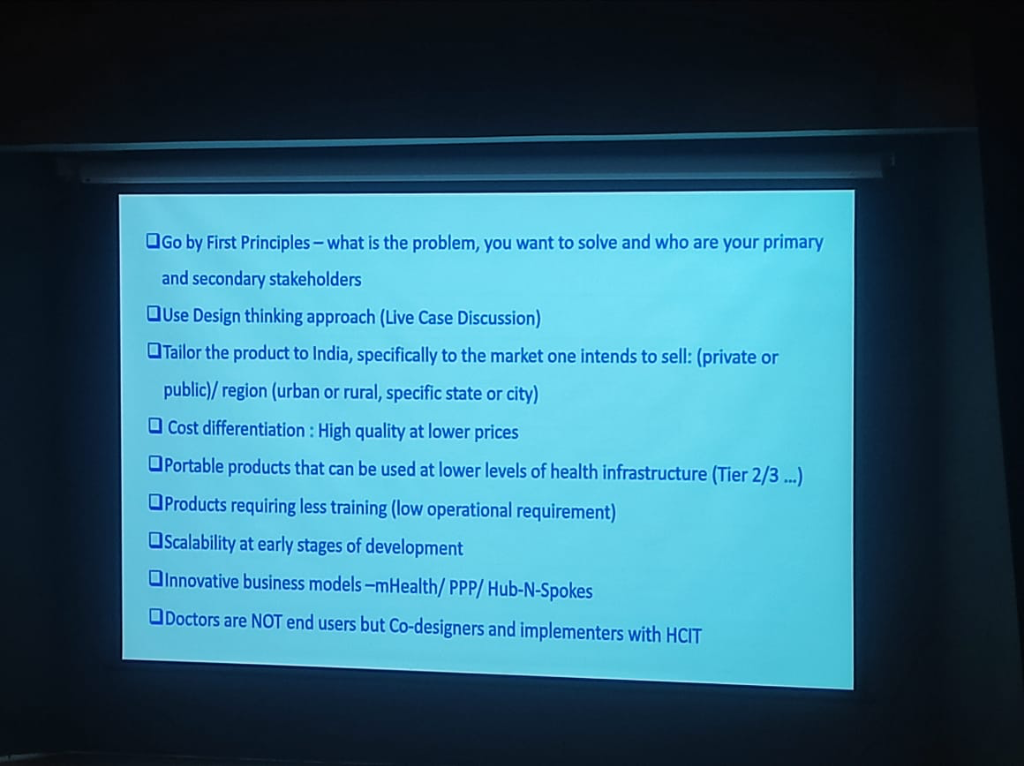 Figure: The design thinking framework for tailoring healthcare products to the Indian market.
Figure: The design thinking framework for tailoring healthcare products to the Indian market.
- Go by First Principles: Success starts with identifying exactly what problem you want to solve and who the primary and secondary stakeholders (clinicians, patients, administrators) are.
- Tailor to the Market: Products must be specifically adapted for the segment they intend to serve:
- Sector Specific: Different strategies for Public vs. Private sectors.
- Region Specific: Accounting for Urban vs. Rural needs, or specific city/state dynamics.
- The India Vectors: Direct integration of native Languages and the ABHA/ABDM identity stack is no longer optional.
- Cost Differentiation: Achieving high quality at significantly lower prices is the benchmark for Indian innovation.
- Doctors are NOT End-Users: A critical paradigm shift is treating doctors as Co-designers and implementers rather than just passive users.
- Workflow is King: Clinicians will not change their existing workflow to suit an app or developer. The technology must instead bend to the clinical reality.
- The Burden of Choice: If a tool requires a doctor to carry an extra device (e.g., a specific digital pen) or adds friction to an emergency, it will be rejected.
- Portability & Scalability:
- Low Level Infrastructure: Designing portable products that function reliably in Tier 2/3 cities.
- Low Operational Requirement: Minimizing the training burden on the healthcare workforce.
- Early-Stage Scalability: Ensuring the product architecture can scale from Day 1.
National TB Elimination Program: Breaking Taboos with AI
A powerful application of AI discussed during the session is its role in the National Tuberculosis Elimination Program (NTEP), where technology is being used to address both clinical and social challenges.
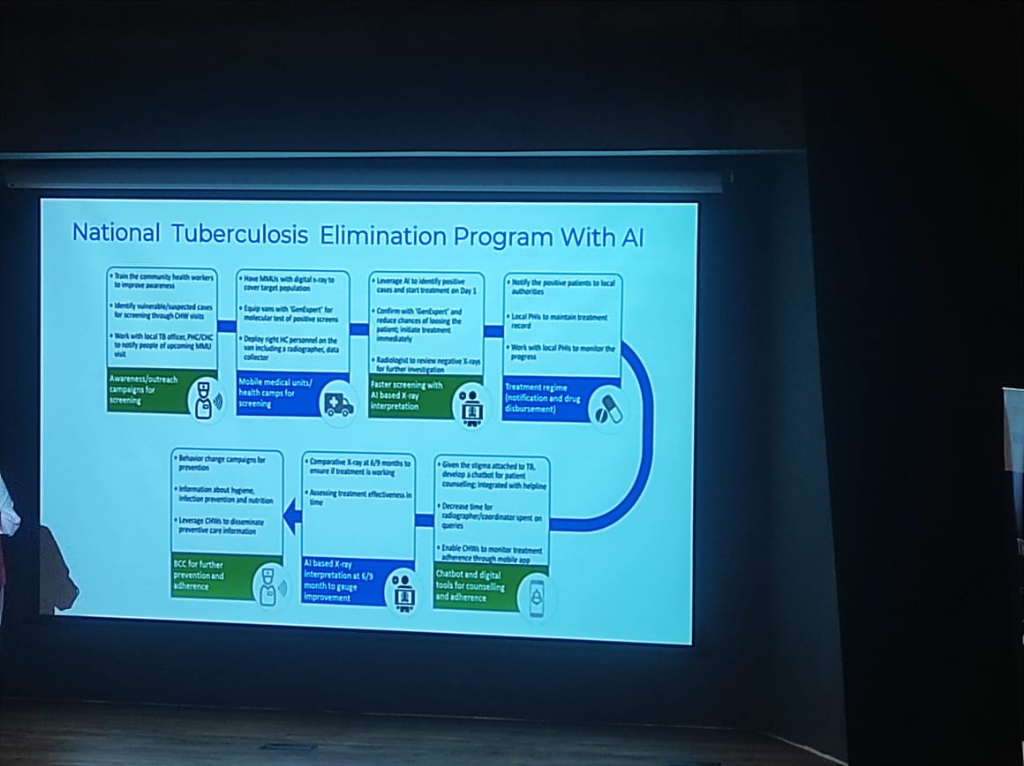 Figure: The AI-driven workflow for national TB elimination, from mobile screening to Day 1 treatment.
Figure: The AI-driven workflow for national TB elimination, from mobile screening to Day 1 treatment.
- AI-Driven Workflow:
- Mobile Medical Units (MMUs): Vans equipped with digital X-rays and AI-based X-ray interpretation software for faster screening.
- Day 1 Treatment: AI identified positive cases are confirmed via GenExpert molecular tests, aiming for treatment initiation on the very first day.
- Continuous Oversight: AI is used to review negative X-rays for further investigation and to gauge improvement via comparative X-rays at 6/9 months.
- Breaking the Stigma: The Trilingual Chatbot:
- The Taboo Challenge: TB carries a significant social stigma in many communities, often leading to delayed treatment.
- The AI Solution: A trilingual chatbot (supporting 3 languages) was developed for patient counseling and adherence.
- Outcome: Patients were found to be significantly less hesitant to interact with a bot than with a human for TB queries, bypassing the taboo and ensuring better engagement.
- Support Tools: The workflow incorporates Differential Diagnosis for lung conditions, Doc Scanners for digital records, and BCC (Behavior Change Communication) campaigns to improve awareness.
Phygital Delivery: Bridging the Last Mile
A core theme of the transformation is the Phygital (Physical + Digital) model, which acknowledges that technology alone is insufficient in the Indian context without a robust physical touchpoint layer.
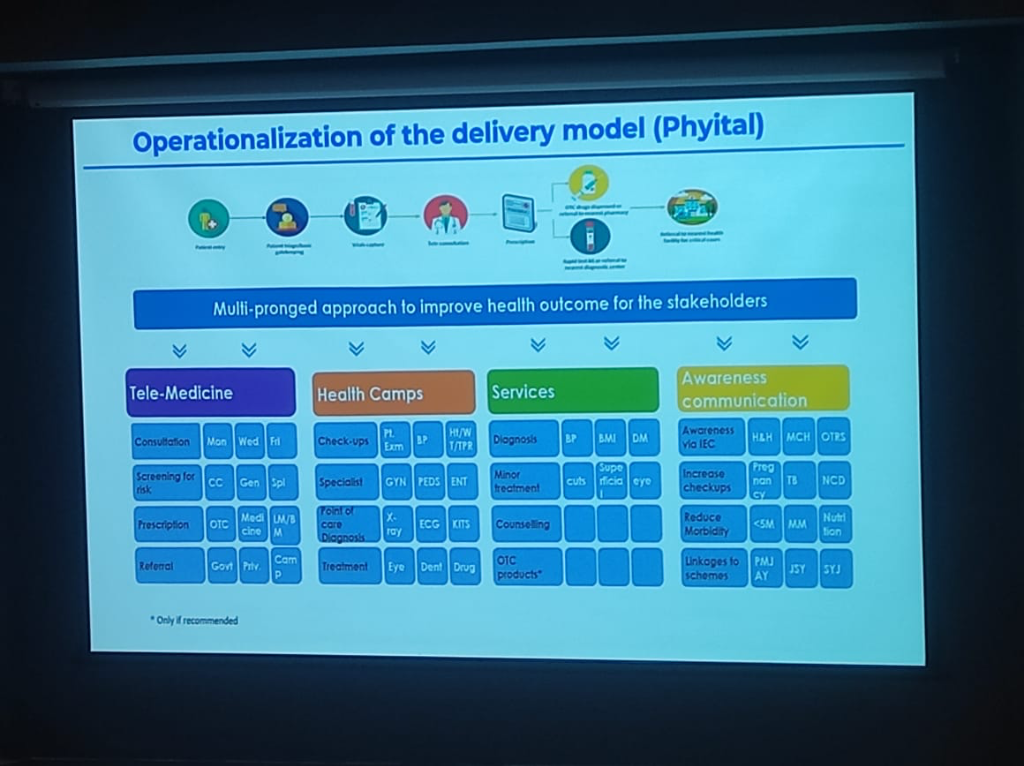 Figure: Operationalization of the Phygital delivery model, integrating community health gates with digital consultations.
Figure: Operationalization of the Phygital delivery model, integrating community health gates with digital consultations.
- The Phygital Patient Journey:
- Community Gatekeeping: The journey begins with Anganwadi and ASHA workers who act as the primary physical triage layer.
- Vitals & Triage: Patient information and vitals are captured at the community level before escalation.
- Digital Bridge: Tele-medicine connects these community hubs to specialists, ensuring that distance is no longer a barrier to quality care.
- Point-of-Care Diagnosis: Rapid test kits and referrals to nearest diagnostic centers complete the loop.
- Service Pillars:
- Tele-Medicine: Continuous consultation and risk screening.
- Health Camps: Periodic physical check-ups and specialist screenings.
- Diagnostic Services: Basic lab work and minor treatments delivered locally.
- Awareness Communication: IEC (Information, Education, and Communication) campaigns focused on Maternal and Child Health (MCH), Nutrition, and non-communicable diseases (NCDs).
Industry Trends 2021-2030: The Digital Explosion
Dr. Prabhu provided a forward-looking roadmap for the Indian healthcare market, projecting a decade of unprecedented growth.
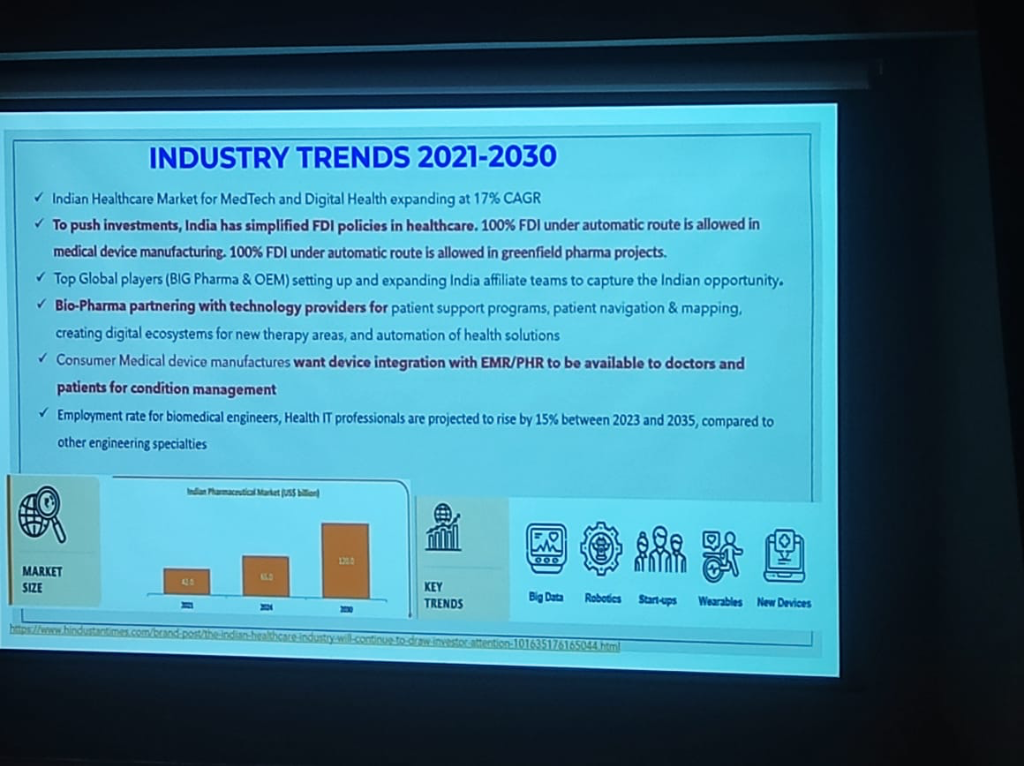 Figure: Key trends shaping the Indian healthcare landscape through 2030.
Figure: Key trends shaping the Indian healthcare landscape through 2030.
- 17% CAGR Growth: The market for MedTech and Digital Health is expanding at a robust 17% compound annual growth rate.
- Investment Simplification: India has simplified FDI policies, allowing 100% FDI under the automatic route for medical device manufacturing and greenfield pharma projects.
- Global Affiliate Expansion: Top global players (BIG Pharma & OEMs) are expanding their India-based teams to capture this regional opportunity.
- Tech-Pharma Partnerships: Bio-Pharma is increasingly partnering with technology providers for patient support programs, navigation, and therapy-area automation.
- The Talent Surge: Employment for biomedical engineers and Health IT professionals is projected to rise by 15% (2023-2035), outpacing most other engineering specialties.
The Reality of Gaps: Infrastructure & Human Capital
Despite the growth, the session highlighted the sheer scale of the challenges remaining in the Indian ecosystem.
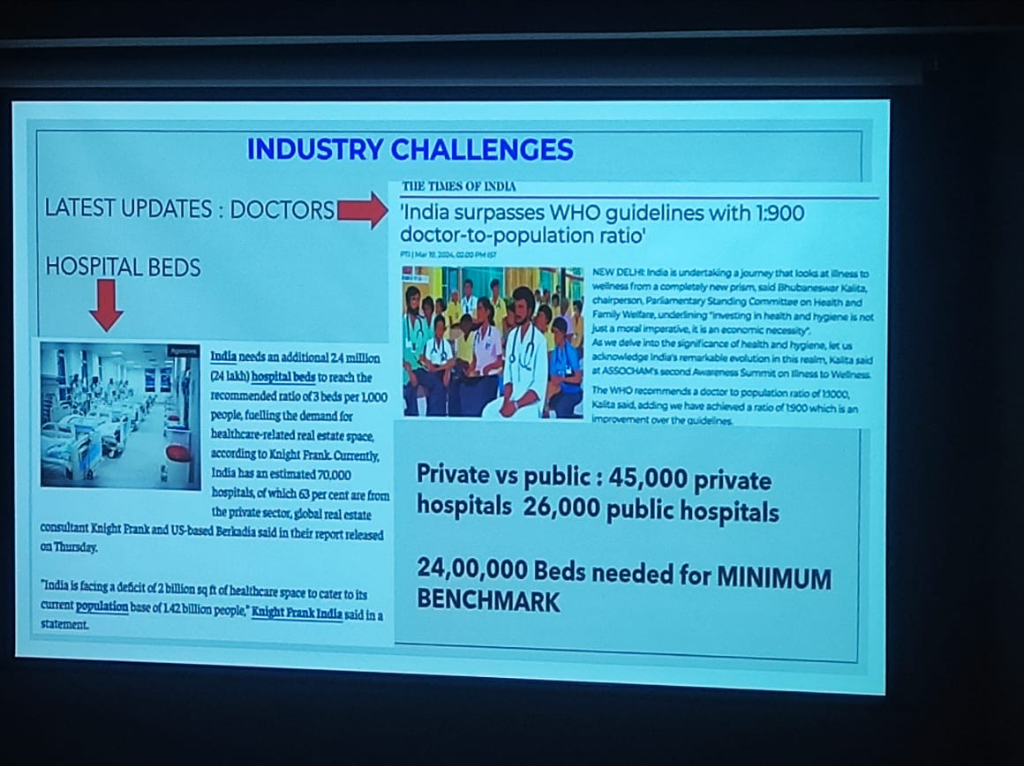 Figure: The infrastructure and human capital gaps in Indian healthcare.
Figure: The infrastructure and human capital gaps in Indian healthcare.
- The Bed Deficit: India needs an additional 2.4 million (24 lakh) hospital beds to reach the recommended ratio of 3 beds per 1,000 people.
- Doctor Ratios: India has recently surpassed the WHO guideline of 1:1,000 with a 1:900 doctor-to-population ratio, a significant milestone, though distribution remains a challenge.
- Sector Split: The landscape is dominated by 45,000 private hospitals vs. 26,000 public hospitals, emphasizing the need for private sector integration into national digital missions.
Investment Tailwinds: PE & M&A Activity
The strategic importance of Indian healthcare is reflected in the massive capital flows into the sector between 2022 and 2024.
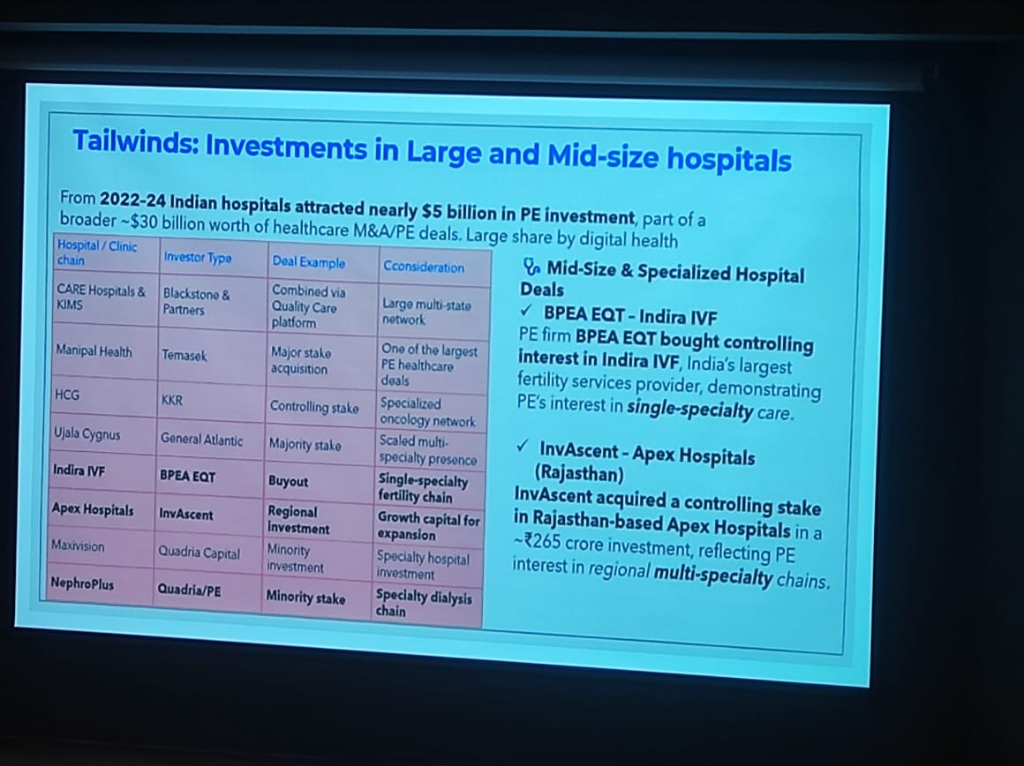 Figure: The landscape of Private Equity and M&A deals in Indian healthcare (2022-2024).
Figure: The landscape of Private Equity and M&A deals in Indian healthcare (2022-2024).
- PE Influx: Indian hospitals attracted nearly $5 Billion in PE investment over the last two years.
- M&A Volume: A broader $30 Billion worth of healthcare M&A and PE deals were recorded, with a significant share driven by digital health integration.
- Strategic Consolidation: Major deals include Blackstone's acquisition of CARE Hospitals/KIMS and Temasek's major stake in Manipal Health.
- Specialized Growth: PE firms like BPEA EQT and InvAscent are focusing on single-specialty chains (e.g., Indira IVF) and regional multi-specialty platforms.
Digital Health Models: From Horizontal Scale to Clinical Trust
The Indian ecosystem is witnessing a diverse range of digital health applications, from broad platforms to trust-driven specialized models.
- Horizontal Scale & Profitability (e.g., Practo):
- Market Success: Practo is a primary example of a horizontal health platform that has achieved significant scale, gone public, and reached profitability.
- Core Offering: Focused on doctor discovery, appointment booking, and digital prescription infrastructure across a wide range of specialties.
- Crowdsourced Clinical Trust (e.g., Lybrate):
- Crowdsourced Intelligence: Lybrate specializes in providing second opinions through a crowdsourced model.
- Peer-Reviewed Trust: Its unique value proposition lies in the peer review of medical opinions, building a "trust layer" that navigates clinical uncertainty.
- Specialized Engagement: Unlike horizontal platforms, it focuses on high-intent clinical queries and peer-validated medical insights.
Innovative Operational Models
To succeed in this environment, innovation must move beyond product-level technology to encompass service delivery and operating models.
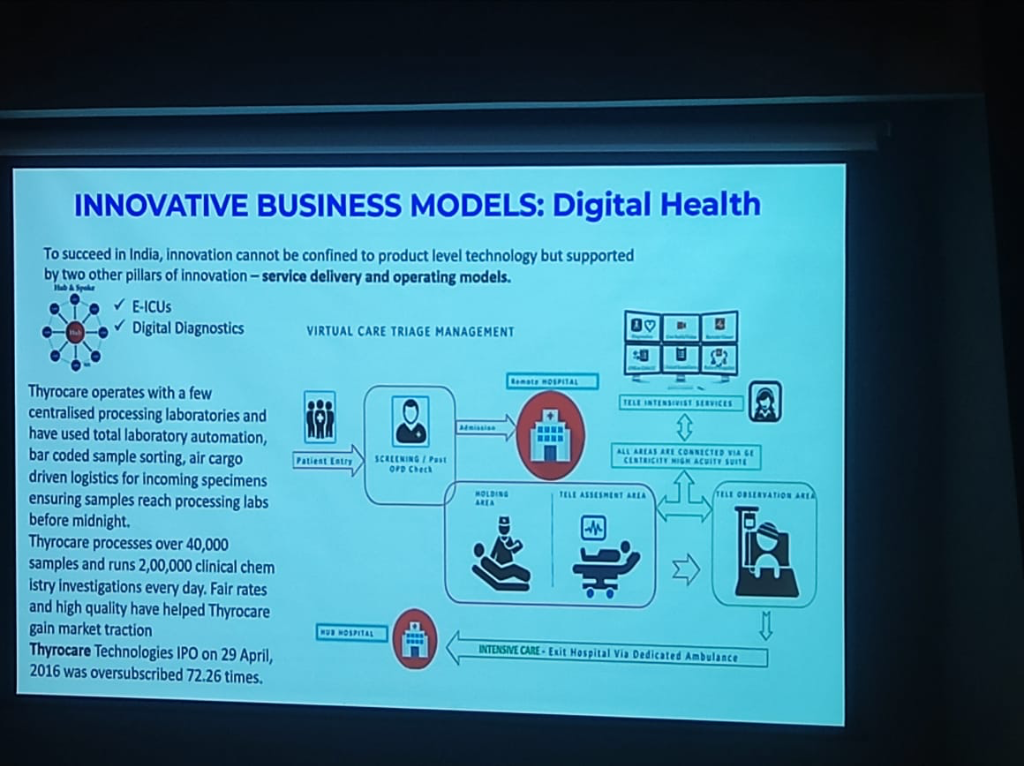 Figure: Innovative business and operating models in the digital health ecosystem.
Figure: Innovative business and operating models in the digital health ecosystem.
- Centralized Hub-Spoke Lab Model (e.g., Thyrocare):
- Hub-Spoke Architecture: A massive decentralized network of collection points (spokes) feeding into centralized processing hubs.
- Overnight Processing: Utilizing air cargo-driven logistics to ensure specimens reach one of the 4 centralized processing hubs by midnight.
- Total Automation: Implementing bar-coded sample sorting and end-to-end automated clinical chemistry paths.
- Scale & Efficiency: Processing over 200,000 investigations daily, proving that high-quality diagnostics can be delivered at fair rates through massive scale.
- Virtual Care Triage (e.g., GE Centricity):
- Remote Triage: Implementing Tele-ICU hub-and-spoke models where local teams are supported by remote specialists via high-acuity suites.
- MIoT Integration: Utilizing the Medical Internet of Things for continuous oversight of vitals and imaging across regional networks.
Business Thinking: The Value Creation Shift
A profound takeaway from Dr. Prabhu's session was that Digital Transformation is not an IT project. It is an organizational, financial, and cultural shift aimed at Value Creation.
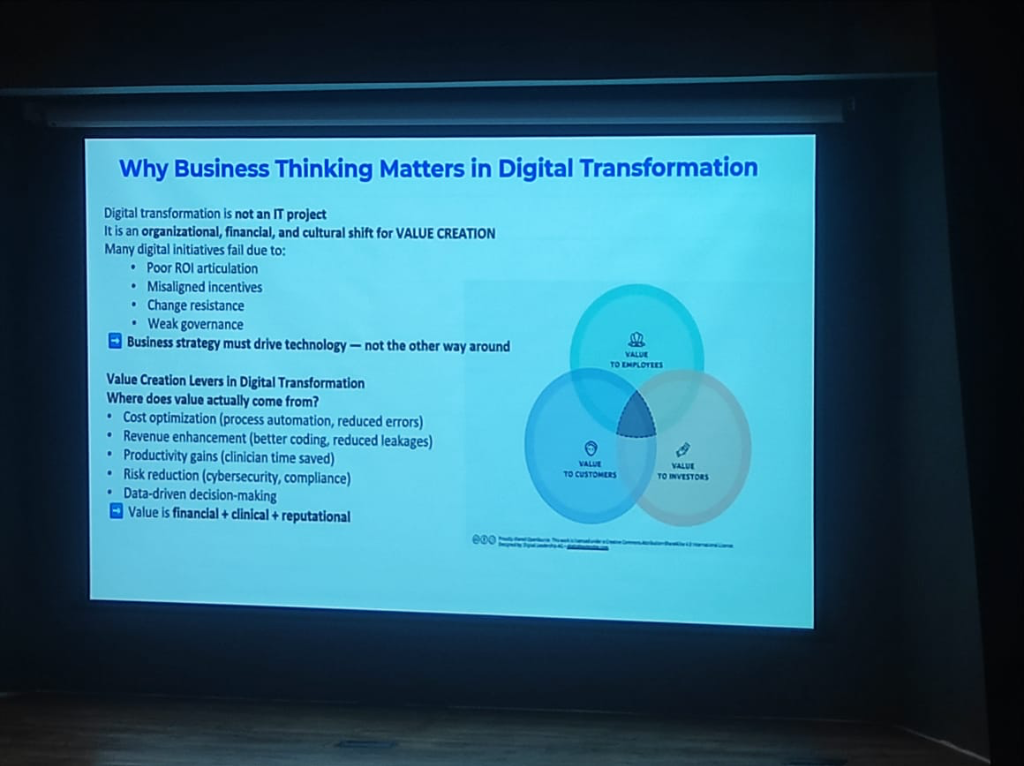 Figure: The value creation levers in digital transformation, bridging employees, customers, and investors.
Figure: The value creation levers in digital transformation, bridging employees, customers, and investors.
- Why Initiatives Fail: Many digital projects falter because of poor ROI articulation, misaligned incentives, change resistance, or weak governance.
- Value Creation Levers: True value in digital health comes from:
- Cost Optimization: Process automation and reduced clinical errors.
- Revenue Enhancement: Better coding and reduced leakages.
- Productivity Gains: Saving precious clinician time.
- Risk Reduction: Ensuring cybersecurity and regulatory compliance.
- The Value Triad: Value must be measured across three dimensions: Financial, Clinical, and Reputational.
Hospital Reality Check: Aligning Strategy with Goals
Dr. Prabhu provided a "Reality Check" for innovators, highlighting the common ground realities that every digital strategy must address.
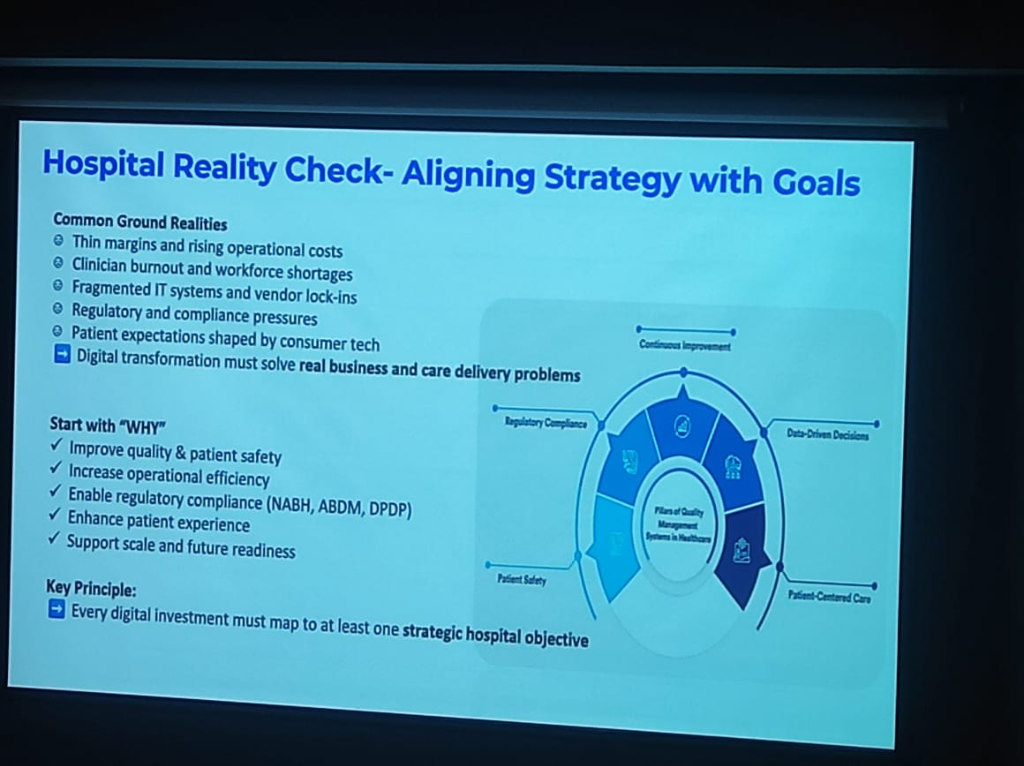 Figure: Aligning digital strategy with strategic hospital objectives and operational realities.
Figure: Aligning digital strategy with strategic hospital objectives and operational realities.
- The Challenges: Hospitals operate under thin margins, rising costs, clinician burnout, fragmented IT systems, and intense regulatory pressure.
- Start with "WHY": Every digital investment must map to at least one strategic hospital objective:
- Quality & Patient Safety: Improving clinical outcomes.
- Operational Efficiency: Streamlining workflows.
- Compliance: Adhering to standards like NABH, ABDM, and the DPDP Act.
- Patient Experience: Meeting the expectations shaped by modern consumer tech.
- Key Principle: Strategy must drive technology—not the other way around. Having the right information at the right time is the ultimate goal of clinical digitization.
Thanga Prabhu Session: Launching the National Awareness Campaign
A landmark moment at KCDH, IIT Bombay was the session led by Dr. Thanga Prabhu (MBBS, Emergency Medicine Specialist, former CMIO for Apollo Hospitals). With over a decade of experience in Emergency Medicine across Abu Dhabi and the UK, Dr. Prabhu brought a global clinician's perspective to the inauguration of the pan-India awareness campaign for the Ayushman Bharat Digital Mission (ABDM).
- The Bahubali Metaphor: Dr. Prabhu opened with the image of the GSLV Mark III, popularly known as "Bahubali"—India's heaviest rocket. This was not just a tribute to space exploration, but a metaphor for India's massive technical capability. ABDM is envisioned as a similar "moonshot" for healthcare.
- Make in India: Engineering Self-Reliance: A core message was the shift toward absolute self-reliance. India no longer needs to import digital health infrastructure. Just as the country built the Param Supercomputer when denied foreign technology, it is now building its own health-tech ecosystem. India is now the "Manufacturing and Engineering Capital" for the world.
- The Trust Deficit: A critical "trust deficit" currently faces the private healthcare ecosystem. When patients visit private facilities today, there is often uncertainty about whether a procedure is for the patient's benefit or the hospital's bottom line.
- The Rethink of Healthcare: ABDM represents a complete rethink of the ecosystem. Just as the government took responsibility for education and healthcare through institutions like IIT and AIIMS, it is now building the digital infrastructure to restore trust and transparency.
Interoperability: The Technical Foundation
A key technical pillar discussed by Dr. Prabhu is the role of standardized interoperability through the National Resource Centre for EHR Standards (NRCES) and CDAC.
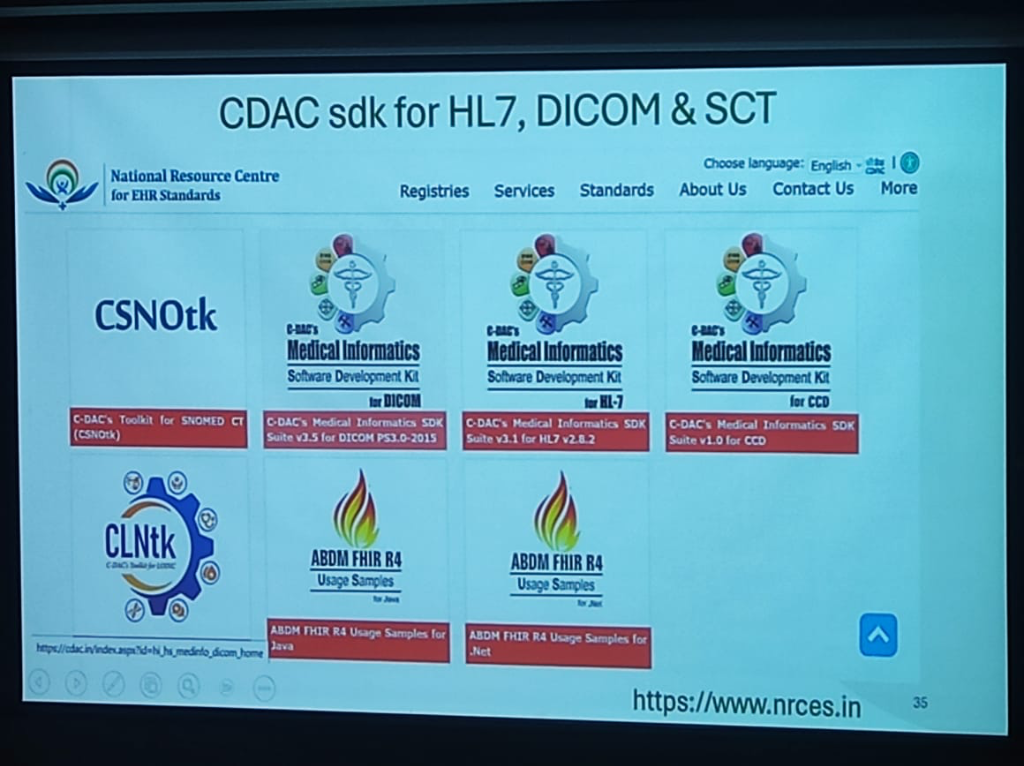 Figure: The CDAC Medical Informatics SDK Suite for HL7, DICOM, and SNOMED CT.
Figure: The CDAC Medical Informatics SDK Suite for HL7, DICOM, and SNOMED CT.
To achieve seamless data exchange across the national health ecosystem, a suite of standardized toolkits has been made available to developers: - CSNOtk: C-DAC's Toolkit for SNOMED CT, enabling standardized clinical terminology across all electronic records. - Medical Informatics SDK Suite: - DICOM PS3.0-2015: For standardized medical imaging and communication. - HL7 v2.8.2: The benchmark for electronic health information exchange. - CCD (v1.0): For Continuity of Care Documents. - ABDM FHIR R4 Usage Samples: To accelerate integration with the Ayushman Bharat Digital Mission, official usage samples are provided for both Java and .Net environments. - CLNtk: C-DAC's Toolkit for LOINC, standardizing laboratory and clinical observations.
These tools, hosted at www.nrces.in, provide the necessary "Lego blocks" for startups and established players to build ABDM-compliant healthcare applications.
Ayushman Arogya Mandirs: The Primary Care Network
India is transforming its primary healthcare through a massive, 400,000-node network, operating under the supreme tagline: "Arogyam Paramam Dhanam" (Health is the Supreme Wealth).
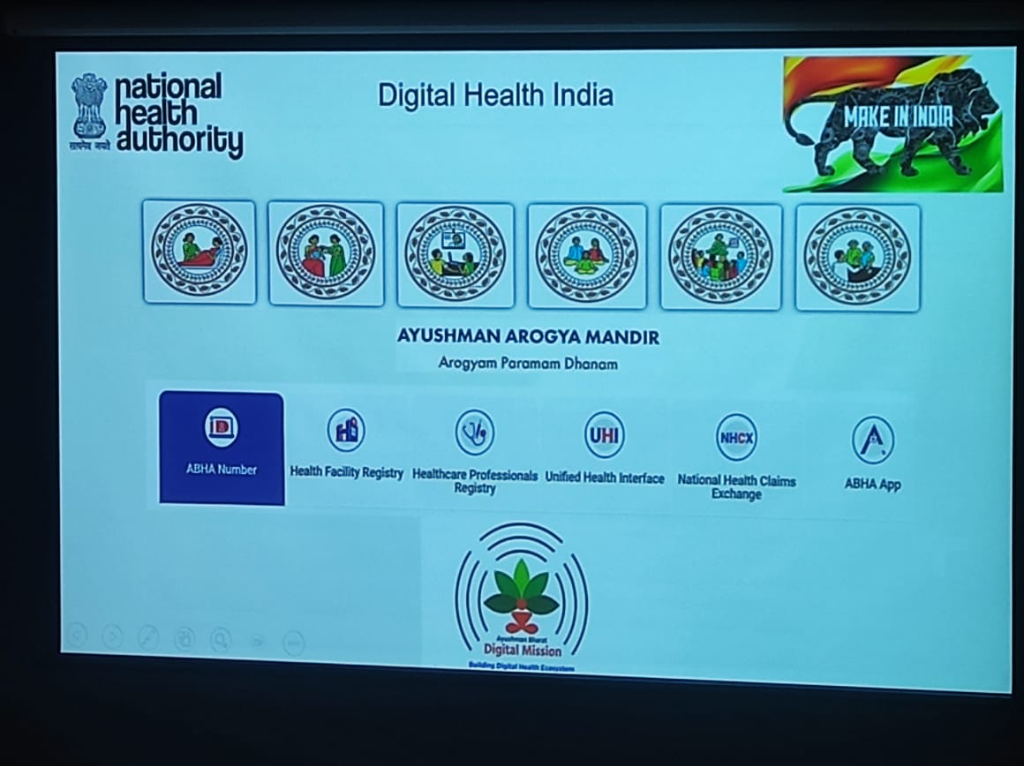 Figure: The National Health Authority's architectural vision for Digital Health India, showcasing the Ayushman Arogya Mandir pillars and the national digital backbone.
Figure: The National Health Authority's architectural vision for Digital Health India, showcasing the Ayushman Arogya Mandir pillars and the national digital backbone.
-
The Six Pillars of Frontline Care: The Arogya Mandir framework is visualized through six core service categories:
- Maternal Health: Comprehensive care for pregnancy and childbirth.
- Child Health: Neonatal, infant, and adolescent care.
- Tele-consultation: Bringing specialized care to remote areas via digital links.
- Reproductive Health: Family planning and reproductive services.
- Communicable Diseases: Management of common infectious diseases and outpatient care.
- NCD & Wellness: Screening and management of non-communicable diseases, alongside yoga and community wellness.
-
Transition from PHCs: What started as 25,000 Primary Health Centers (PHCs) at independence has evolved into 400,000+ Ayushman Arogya Mandirs (formerly Health and Wellness Centers).
- The Geriatric Priority: In a move that addresses a globally neglected segment, India's new primary care framework places a dedicated focus on Geriatric Medicine (60+ care). While the world often ignores the elderly, the Indian model integrates them into the frontline digital health loop.
The National Digital Backbone
Supporting these frontline "Mandirs" is a robust set of five digital pillars defined by the National Health Authority (NHA): - ABHA Number: The unique digital identity for citizens. - Health Facility Registry (HFR): The master database of verified healthcare facilities. - Healthcare Professionals Registry (HPR): The directory of verified doctors, nurses, and paramedical staff. - Unified Health Interface (UHI): The open protocol for digital health services (the "UPI of health"). - National Health Claims Exchange (NHCX): The gateway for seamless, paperless health insurance claims.
Ecosystem Triangulation: ABHA, DigiLocker, and Discovery
A critical architectural nuance shared during the session was the "Triangulation" model of the ABDM ecosystem, which solves the paradox of data storage versus real-time access.
- ABHA (Identity): Provides the persistent, across-the-board identity that anchors a citizen's longitudinal health story.
- DigiLocker (Verification): Acts as the secure, government-verified repository for static "credentials" (e.g., insurance policies, vaccination certificates, and academic degrees).
- Discovery Layer (PHR/HIE): Enables the real-time "discovery" and fetch of dynamic clinical records (e.g., lab reports, discharge summaries, and prescriptions) from disparate hospital nodes.
The Evolution of Clinical Data Entry
A transformative theme of the session was the shift away from traditional, cumbersome data entry toward intelligent, machine-driven workflows.
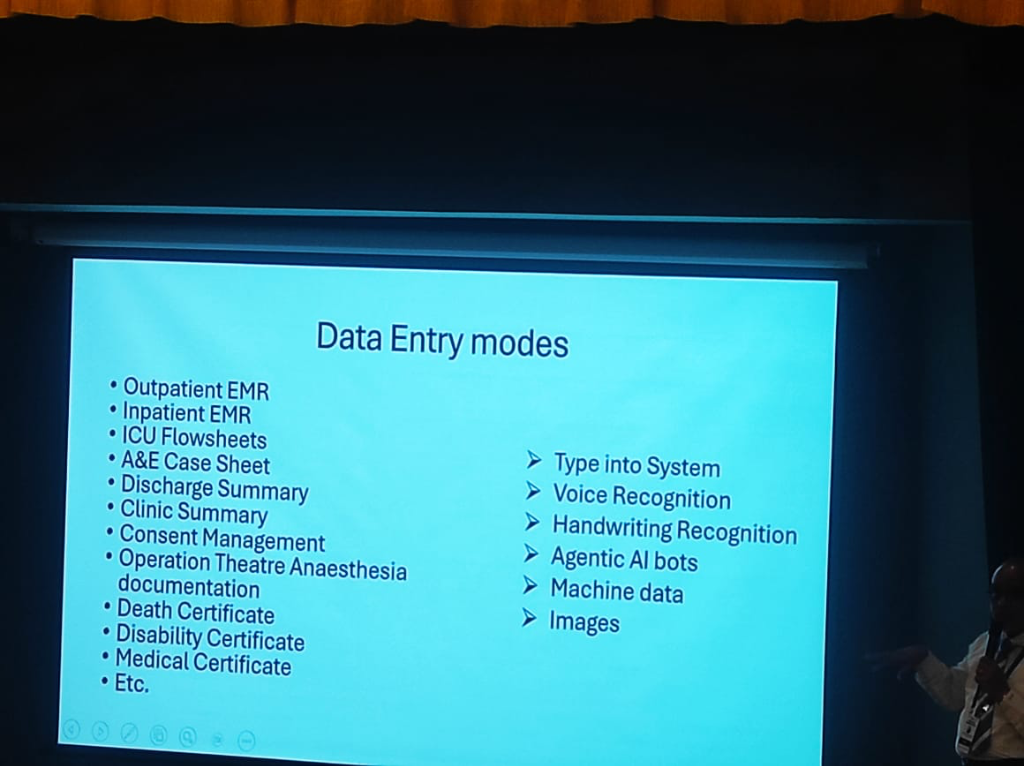 Figure: The transition from manual typing to Agentic AI and machine data in clinical environments.
Figure: The transition from manual typing to Agentic AI and machine data in clinical environments.
- The Document Spectrum: Dr. Prabhu highlighted the diverse array of complex clinical documents that require digitization to build a true longitudinal history:
- Acute Care: A&E Case Sheets, ICU Flowsheets, and OT Anaesthesia documentation.
- Certifications: Death, Disability, and Medical Certificates.
- Routine Care: Outpatient/Inpatient EMRs, Discharge and Clinic Summaries, and Consent Management.
- The Entry Modes: The roadmap moves beyond the "Type into System" era, embracing:
- Vendor Case Examples:
- Voice (Augnito): Grounding the vision of voice-first clinical workflows by referencing Augnito's high-accuracy, real-time medical dictation.
- Handwriting (DocsPro Pen): Utilizing the DocsPro Digital Pen as the bridge between paper-based workflows and digital data. However, this mode faces real-world adoption hurdles: doctors are reluctant to carry a second pen and fear the fragility of the device in high-pressure clinical moments.
- Rounds Notes (DailyRounds): Positioning DailyRounds as a specialized enterprise app for doctor rounds notes. In the "post-eSushrut" (C-DAC HMIS) era, such apps serve as a critical second layer, capturing deep clinical nuances and providing a superior user experience for bedside documentation that broad-based systems may miss.
- Machine Data & Images: Direct ingestion from medical devices and diagnostic imaging.
- Agentic AI Bots: Dr. Prabhu specifically identified Agentic AI as the primary future mode for data entry. This represents a fundamental shift from "typing into a system" to having autonomous agents that assist in capturing, structuring, and verifying clinical data in real-time.
Agentic AI: A New Vision for Hospital Operations
One of the most forward-looking themes of the session was the definition of Agentic AI and its role in fundamentally transforming how hospital systems work.
Current Systems vs. The Agentic Shift
Traditional hospital systems (HIS/EMRs) are historically static gateways. They require high manual effort to "input" data and often act as digital filing cabinets that respond only to direct human commands.
In contrast, Agentic AI represents a shift toward: - Autonomy: Systems that don't just store data but take proactive actions based on clinical goals. - Real-Time Orchestration: Moving from periodic "data entry" to a continuous flow of assistance that moves with the surgical or clinical team. - Why it's Different: Unlike previous AI generations that were purely analytical (identifying patterns), Agentic AI is operational—it can navigate workflows, coordinate between departments, and assist in real-time decision-making.
The Three Pillars of Agentic Operations
The vision for the future hospital is built on three core operational principles:
- Intelligent: The system provides more than just data storage; it offers real-time insights and automated orchestration of the patient journey.
- Adaptive: The technology is designed to thrive in the dynamic, high-pressure environment of a hospital. It adjusts to emergencies, resource shifts, and changing clinical priorities in real-time.
- Human-Centric: Most importantly, the technology is built around the humans who use it. It aims to reduce the "operational load" on clinicians, allowing them to focus on the patient rather than the screen.
Smart OT & TeleICU: The High-Tech Clinical Core
Dr. Prabhu shared a deep dive into the high-capital, high-tech environments where digital integration is most critical.
-
Smart OT (Operation Theatre):
- Interconnectivity: Modern OTs feature interconnected systems where real-time data feeds from surgical equipment are automatically captured into the electronic surgical record (ESR).
- IoT & Sensors: The environment is heavily instrumented with IoT sensors and AI analytics to optimize surgical workflows and patient safety.
- Remote Assistance: Digital imaging and tele-medicine allow for real-time remote assistance from specialists during complex procedures.
-
TeleICU: Scalable Critical Care:
- The Hub-and-Spoke Model: A central Tele-ICU hub can support multiple hospitals across different regions, extending specialized critical care expertise to facilities that lack full-time intensivists.
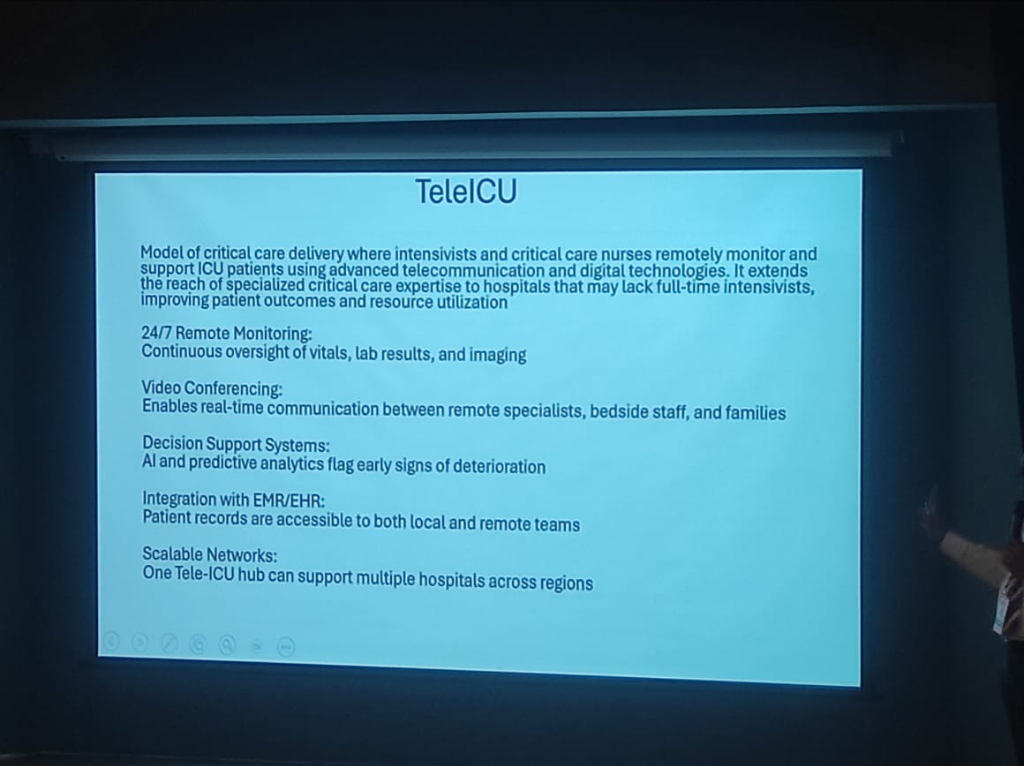 Figure: The architecture of a scalable TeleICU network, featuring remote monitoring and AI decision support.
Figure: The architecture of a scalable TeleICU network, featuring remote monitoring and AI decision support.
- 24/7 Monitoring: Intensivists and nurses remotely monitor vitals, lab results, and imaging data around the clock.
- AI Decision Support: Advanced analytics and predictive AI flag early signs of patient deterioration, allowing for proactive intervention.
- Video Collaboration: Enables real-time communication between remote specialists, bedside staff, and families.
Specialized Systems: LIMS & AI Radiology
The digitization of clinical ecosystems is completed by specialized, high-fidelity systems. - LIMS (Laboratory Information Management): These systems manage the entire lifecycle of a medical laboratory—from sample tracking and testing to processing and reporting—ensuring end-to-end data integrity. - AI in Radiology (PACS/RIS): The radiology field is highly mature in its use of AI. Images captured via PACS (Picture Archiving and Communication System) are now routinely interpreted by AI algorithms to generate high-accuracy preliminary reports, freeing up radiologists for more complex cases.
NHCX: The 30-Second Claim
A major breakthrough in the ABDM architectural roadmap is the National Health Claims Exchange (NHCX). - The Efficiency Goal: Currently, insurance claims are bogged down by manual verification and paper-heavy workflows. NHCX aims to transform this into a 30-second automated approval flow. - The "UPI" for Claims: By triangulating Identity (ABHA) and Eligibility (Insurance credentials in DigiLocker), NHCX allows for near-instant validation of clinical necessity and coverage, drastically reducing the "Trust Deficit" between providers, patients, and payers.
The Indian Healthcare Duality
Dr. Prabhu provided a structural overview of the two-speed healthcare system that ABDM serves, anchored in a stark contrast between the public and private sectors.
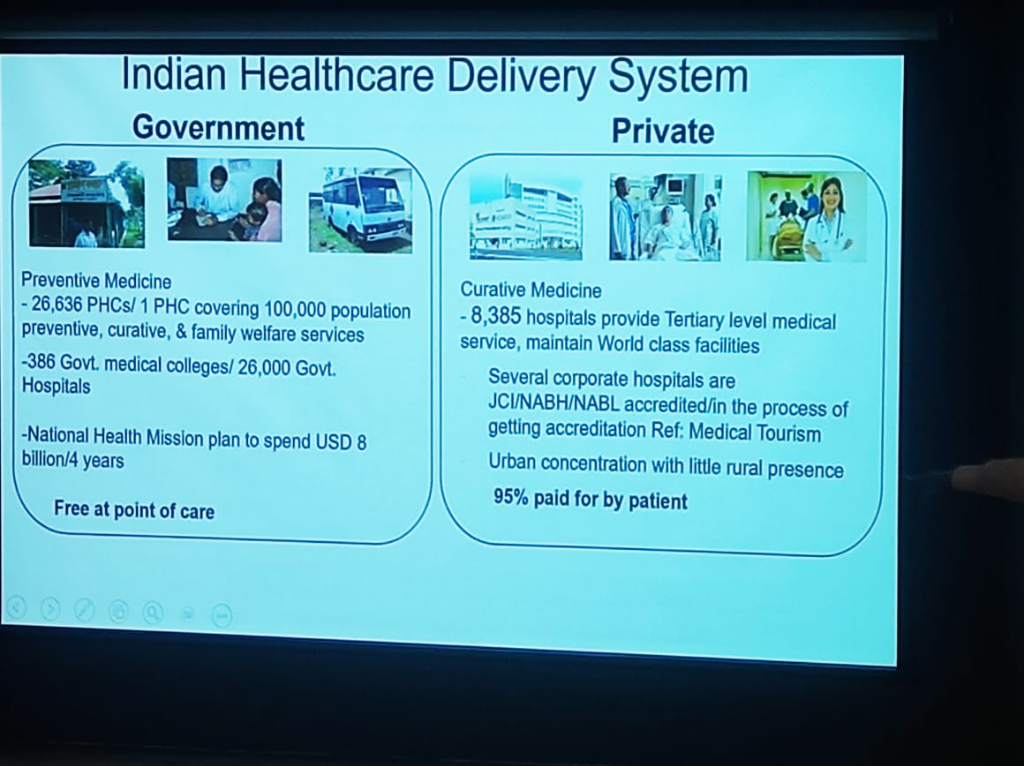 Figure: The structural contrast between Government (Preventive-First) and Private (Curative-First) healthcare delivery in India.
Figure: The structural contrast between Government (Preventive-First) and Private (Curative-First) healthcare delivery in India.
- Private Healthcare (Curative-First):
- Scale: Comprises 8,385 tertiary hospitals providing world-class medical services.
- Accreditation: Many are JCI/NABH/NABL accredited, positioning India as a global hub for medical tourism.
- The Gap: Despite its excellence, the sector has a heavy Urban Concentration with little rural presence.
- The Cost: A staggering 95% of costs are paid for by the patient, a financial burden that ABDM’s transparency and NHCX integration aim to mitigate.
Corporate Healthcare Dynamics
The private sector in India is evolving from traditional "hospitals" toward a model of "Hospitality in Hospitals", focusing on premium patient experience and standardized services.
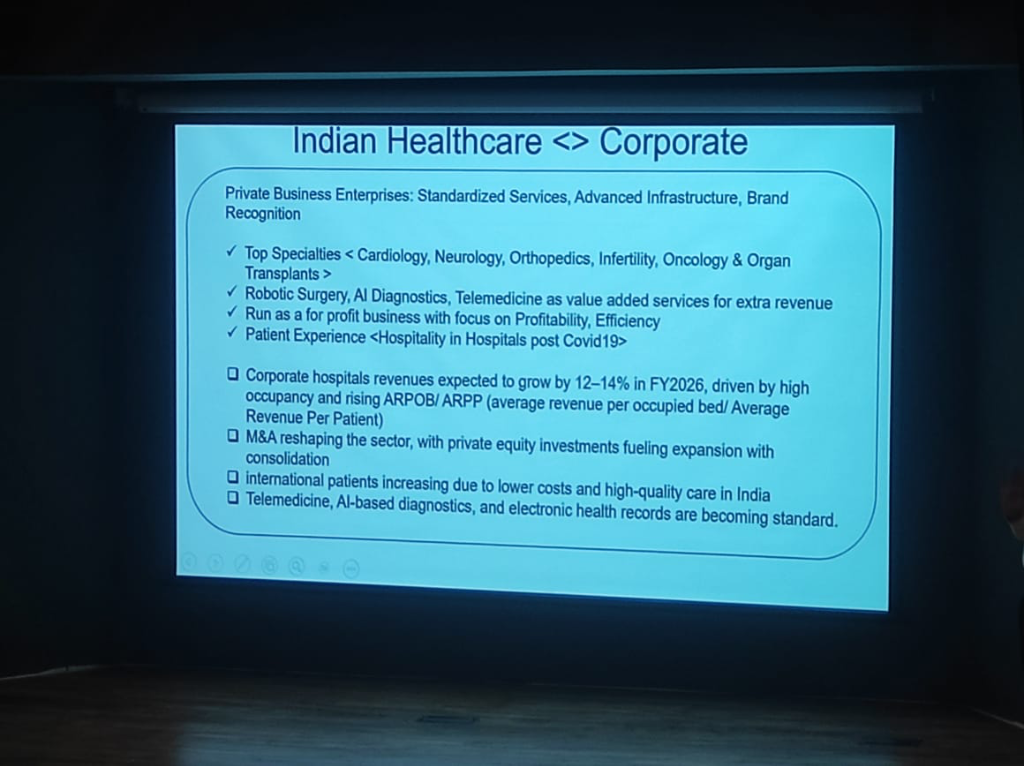 Figure: The operational and financial roadmap for India's corporate healthcare sector.
Figure: The operational and financial roadmap for India's corporate healthcare sector.
- Growth & M&A: The sector is seeing aggressive expansion and consolidation, with revenues expected to grow by 12-14% in FY2026, driven by high occupancy and rising ARPOB/ARPP (Average Revenue Per Occupied Bed/Patient).
- The Telemedicine Behavior Shift: Post-COVID, there has been a fundamental behavioral shift. The "remote culture" has moved Telemedicine from a backup option to a standard "value-added service." It is now an integral part of the patient experience and a key revenue engine.
- Revenue Engines: The sector is pivoting toward high-specialty services (Cardiology, Neurology, Oncology) and adopting high-tech drivers like Robotic Surgery and AI Diagnostics to maintain profitability and efficiency.
- Electronic Health Records: Integration with ABDM is becoming a standard requirement for private business enterprises to maintain brand recognition and operational parity.
Global Context: System Failures and Monopoly Risks
Dr. Prabhu provided a sobering comparison between India's emerging digital ecosystem and the established systems in the West.
- Western System Failures:
- United States: The system is widely perceived as failing due to the massive overhead and inefficiencies driven by the insurance-first model, which prioritizes payer-provider negotiations over patient outcomes.
- United Kingdom (NHS): While conceptually sound, the NHS is currently struggling with severe bottlenecks in access to doctors, with patients facing months-long waits for standard appointments and procedures.
- The Monopoly Risk: A recurring theme in the session was the caution regarding Mergers and Acquisitions (M&A) in the Indian private sector. While consolidation can drive efficiency, it also brings the risk of monopolies, which can stifle innovation, limit patient choice, and drive up costs in the long run.
The Rise of Medical Tourism
Amidst these global challenges, India's tertiary sector is emerging as a global leader in Medical Tourism. - Quality at Scale: By combining international-grade accreditation (JCI/NABH) with high-volume clinical expertise, Indian corporate hospitals provide outcomes comparable to the best in the West. - The Cost Arbitrage: India offers these world-class services at a fraction of the cost found in the US or Europe. This combination of "Top Quality" and "Low Cost" is positioning the country as the definitive global hub for complex medical procedures, further incentivized by the digital transparency brought by ABDM.
By triangulating across these three—Identity (ABHA), Verification (DigiLocker), and Discovery (ABDM)—the mission creates a "trust bridge" that ensures data is verified at the source and accessible at the point of care.
The DNA of Excellence: An Indian Identity
Dr. Prabhu highlighted that the success of the digital mission is rooted in a unique "DNA of Excellence" driven by decades of national investment.
- From Shyness to Pride: While Indians are often "shy by nature" in claiming credit, Dr. Prabhu noted that the world's best companies are now run by Indians. This is the fruit of 30-40 years of deep investment in Education, Medicine, and Engineering.
- The Education Priority: Unlike many Western contexts, India places an unparalleled priority on education. The mantra of "study well and do well" is embedded in the cultural fabric, providing a high-quality human capital baseline for digital transformation.
- Global Leadership: This investment is now yielding fruit across all fields—Pure Science, Engineering, and Medicine—positioning India not just as a consumer of digital health, but as a global leader in its innovation and deployment.
Preventive-First: A Strategic Shift
A core theme of the session was the fundamental shift from curative-only to Preventive-First healthcare.
- The Cure Paradox: While curative medicine—transplants, cardiac procedures, and high-capital neurosurgeries—is necessary, its impact is limited by resources and cost.
- Community-First Care: Dr. Prabhu emphasized that health begins in the community. The strategic goal is to manage health before a person becomes a patient. If managed well in the community, they don't even need to enter the hospital, reducing friction and cost across the entire system.
- Population Health: The real benefit for India's population lies in Primary and Preventive Health. By focusing on lifestyle diseases and early intervention, ABDM aims to keep people out of hospitals rather than just managing them once they are there.
- Standardized Prevention: The digital mission provides the platform to operationalize this preventive strategy at a national scale, making it the "first point" of the whole ecosystem.
Home Healthcare: The Next Frontier
A significant shift highlighted by Dr. Prabhu is the transition from hospital-centric to Home-Centric Care.
- Delivering Care at Home: Technology now enables the management of long-term conditions (Diabetes, Hypertension) and post-acute recovery in the patient's home.
- Palliative & Mental Health: Palliative and end-of-life care, traditionally restricted to hospitals or nursing homes, can now be managed more humanely at home. Similarly, Mental Health services are being successfully delivered remotely.
- The Elderly Opportunity: Dr. Prabhu identified Elderly Care as the "next big opportunity" for the next 50 years—a sector that is currently neglected but holds massive potential for digital innovation.
- Connected Ambulances: By utilizing MIoT (Medical Internet of Things), ambulances are being transformed into "field clinical delivery" units, allowing for life-saving interventions before the patient even reaches the hospital.
Just-in-Time Skills: Rapid Upskilling
The rapid pace of digital transformation requires a fundamental shift in how we approach medical and technical education.
- Beyond the Classroom: The days of spending years in a college to learn a static skill set are over. The fast-moving digital health landscape demands Just-in-Time Skills.
- Real-Time Learning: Professionals must now be able to quickly ramp up on new technologies and protocols as they emerge. This shift toward continuous, real-time upskilling is critical for building the cadre needed to support the digital mission.
ABDM: The Biggest Startup Opportunity
Dr. Prabhu issued a strong call to action for innovators, framing ABDM as the "Biggest Startup Opportunity" in the country today. Drawing on his experience as CMIO, he detailed a structured roadmap for where innovation is most needed.
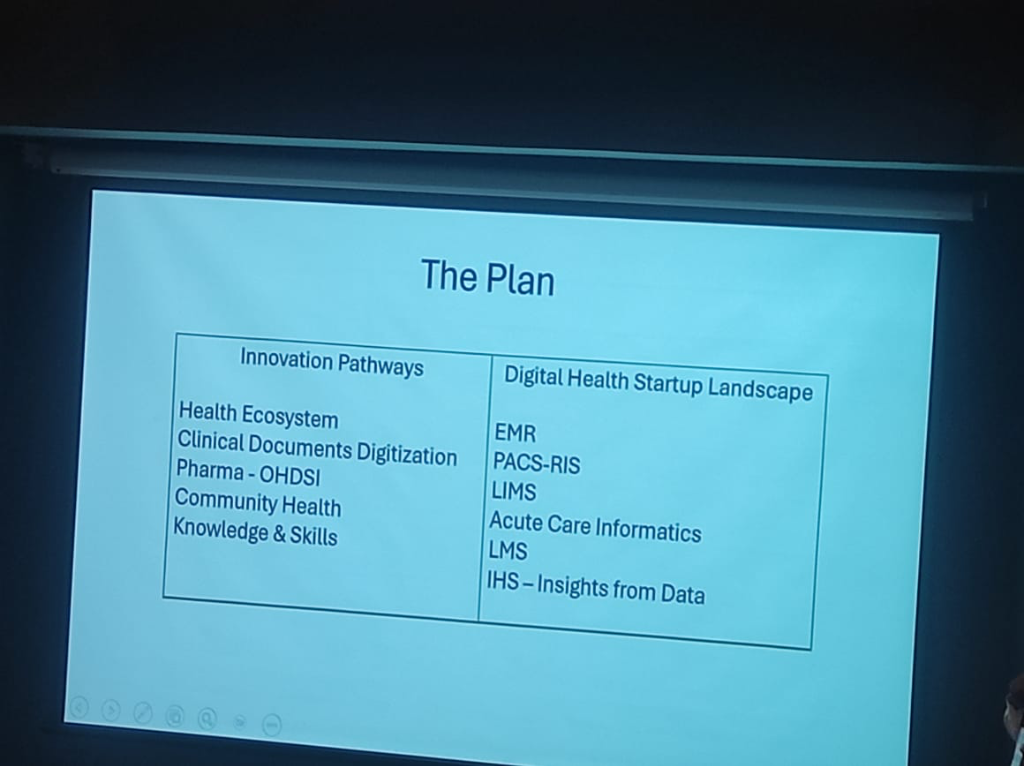 Figure: The strategic plan for digital health innovation pathways and the startup landscape.
Figure: The strategic plan for digital health innovation pathways and the startup landscape.
| Innovation Pathways | Digital Health Startup Landscape |
|---|---|
| Health Ecosystem | EMR (Electronic Medical Records) |
| Clinical Documents Digitization | PACS-RIS (Imaging & Radiology) |
| Pharma - OHDSI | LIMS (Laboratory Info Systems) |
| Community Health | Acute Care Informatics |
| Knowledge & Skills | LMS (Learning Management Systems) |
| IHS (Insights from Data) |
- Innovation at Scale: With 51 innovators already registered at the session's outset, the mission is designed for those who want to solve national problems while building sustainable businesses.
Bioinformatics & The CRO Revolution
Dr. Prabhu detailed how the digitization of health data is fundamentally disrupting the multi-decade drug discovery lifecycle. - Shrinking the 10-Year Window: Traditionally, bringing a drug to market is a 10-year journey. Through Bioinformatics and advanced data management, this window is being significantly compressed. - Clinical Research Organizations (CROs): These organizations act as the execution arm for pharma companies, managing the complex 4-Phase Trial Lifecycle: - Phase 1 & 2: Selecting populations and testing safety/efficacy. - Phase 3 & 4: Post-marketing surveillance once the drug is in the wild. - The Tech Stack: CROs now rely on a sophisticated stack of Clinical Trial Management (CTM), Regulatory Compliance, and Bio-statistics to ensure data integrity and structured reporting.
OHDSI: Standardizing Global Evidence
A cornerstone of the clinical research roadmap is the adoption of OHDSI (Observational Health Data Sciences and Informatics).
- From OMOP to OHDSI: The journey began with the OMOP (Observational Medical Outcomes Partnership), which has now morphed into the international OHDSI (Odyssey) organization.
- Real-World Evidence: OHDSI provides the open-source tools and standardized data models (OMOP Common Data Model) necessary to generate reliable evidence from observational health data across different institutions.
- The OHDSI India Chapter: Recently established (2 years old), this chapter is already collaborating on high-level policy questions from the Government and the WHO—for instance, studying the long-term effects of specific drugs on population health metrics like tuberculosis.
- Predictive Acute Care (Case Study: Coherent): One of the most compelling examples shared was Coherent, a startup focused on ICU automation. By utilizing high-fidelity EMR data, Coherent can predict the onset of Sepsis before it occurs. Sepsis is a condition that kills 60% of ICU patients, and early prediction using digital blueprints is a literal life-saver.
- The Data Payers: Ensuring Sustainability: A critical realization for startups is identifying who pays for these insights. While hospitals are the custodians, the Insurance, Pharma, and MedTech industries are the primary "payers" for high-quality, anonymized clinical data. This insurance-led model ensures the financial sustainability of the digital mission.
- The Triple Bottom Line: Innovators are encouraged to "do well" (build successful products), "solve the country's problems," and "make some money" on the side.
- The Support Ecosystem: The synergy between academic hubs like IIT Bombay (KCDH) and national mission teams creates a blueprint for how technical excellence and public policy can collaborate to support this new wave of health-tech entrepreneurship.
Federated Architecture: Resilience Through Decentralization
A core architectural tenet of the ABDM is the shift from a centralized to a Federated Architecture.
- Decentralized Nodes: Unlike legacy systems where a single point of failure can bring down the entire network, the national backbone is composed of independent, federated nodes.
- Isolating Failure: This design ensures that if a specific facility or region's node is affected—whether by technical downtime or a security incident—it does not hamper the others. The rest of the national ecosystem continues to function seamlessly, ensuring systemic resilience.
- Institutional Autonomy: Facilities maintain control over their data nodes, reinforcing the "Blind-to-Transit" model where the NHA provides the discovery layer without owning the clinical blocks.
The PHR Storage Paradox: Why 1GB Isn't Enough
A critical realization in the national rollout is the storage bottleneck facing Personal Health Record (PHR) applications.
- The DigiLocker Limit: While DigiLocker is a foundational pillar of India's digital infrastructure, it currently provides 1GB of storage. For a lifetime of clinical-grade data—including high-resolution diagnostic imaging and long-term inpatient summaries—this 1GB ceiling is not a viable repository for a comprehensive PHR.
- The "Google Pay" Model for Health: Consequently, the ecosystem is shifting toward a transactional model. Just as Google Pay does not "store" your money but provides a discovery and transaction layer for your bank accounts, modern PHR applications are evolving into Discovery & Transaction Gateways.
- Discovery First: In this model, the PHR app's primary role is to discover records across diverse providers (the "banks") and facilitate their secure, consent-based exchange, rather than serving as a monolithic cloud storage bucket for all clinical assets.
Anonymized Data: The Population Health Asset
While individual records are strictly governed by consent, the mission is unlocking clinical insights at scale through Anonymized Population Data.
- Aggregate Research: Frameworks are being operationalized to make anonymized, aggregated data available for public health research, disease surveillance, and national policy planning.
- Privacy-First Surveillance: By decoupling individual identity from clinical trends, the ecosystem can monitor healthcare efficacy and disease patterns in real-time, creating a national asset for medical research and AI training without compromising privacy.
International Portability: Sovereign Conversations
The vision for Indian digital health extends beyond national borders, aiming for seamless International Portability of health records.
- Ongoing Sovereign Discussions: While the technical baseline (HL7 FHIR) is global, formal cross-border data exchange remains a subject of active Soverign Government Discussions.
- Bilateral Protocols: Integration with international health systems is being negotiated at the diplomatic level to ensure that cross-border integrations are both secure and formally recognized by participating nations.
- Education & Training: NRCeS provides free training—including SNOMED CT courses—to support the whole ecosystem.
- Open Systems & Tools: By providing FOSS tools and libraries, NRCeS address implementation challenges through regular community engagement.
Finalizing National Standards: The NRC Hub
A critical role of the NRC (National Resource Centre for EHR Standards) is finalizing and pushing the HL7 FHIR R4 standards to the country. This ensures that every digital health application in the ecosystem speaks the same semantic language.
The Big Tech Paradox: The Apple Case
A common question in digital health circles is why global giants like Apple are not ABDM compliant. - The Standards Gap: While Apple Health provides a sophisticated personal health record platform, it does not currently adhere to the mandatory HL7 FHIR R4 profiles finalized by the NRC for India. - Proprietary vs. Open: Big Tech's reliance on proprietary data models creates a friction point with national missions that mandate open, interoperable standards for public-private data exchange.
The 7 Core Care Contexts
To ensure granular linkage of clinical encounters, the ABDM framework utilizes Care Contexts. Currently, there are 7 available care contexts that systems must map to:
- OPD Consultation: For standard outpatient visits.
- IPD Admission: For inpatient stays and procedures.
- Diagnostic Test: For lab and imaging results.
- Immunization: For vaccination events.
- Prescription: For digital medication orders.
- Wellness/Health Record: For wearable and telemetry data.
- Pharmacy Invoice: For proof of medication purchase.
The Unique ABHA Constraint: One Person, One ID
A fundamental architectural rule of the national mission is the Uniqueness of the ABHA Number. - No Multiplicity: It is not possible for a single individual to have multiple ABHA numbers. The ID is a unique, life-long identifier anchored to a person's identity. - Single Version of Truth: This constraint ensures that clinical records from fragmented visits are correctly routed back to the same longitudinal history, preventing data silos or duplicate profiles.
Mandatory FHIR R4: The Integration Baseline
For any HIS or EMR to interact with the national HIE, it must undergo a specific type of integration.
- Strict Compliance: ABDM, in collaboration with NRCeS, has mandated HL7 FHIR R4 as the only acceptable standard for data exchange.
- Resource Definition: Whether it's a vaccine certificate or a pharmacy invoice, every HI type is modeled as a FHIR resource (e.g., Patient, Observation, DiagnosticReport), ensuring that data is self-describing and semantically rich.
Success at Scale: IPD Linkage in Bihar
While many states are still focusing on OPD, Bihar has emerged as a leader in complex record linkage. - IPD Record Portability: Bihar has successfully operationalized the linking of In-patient (IPD) records to the ABHA ID. - Live Proof-of-Concept: This demonstrates that even narrative-heavy inpatient summaries can be structured and shared across the national backbone, providing a blueprint for other states to follow.
NHA Auditing & Governance: The Blind-to-Transit Reality
To combat the "shortcut" culture, the NHA and NHM teams are evolving their roles from facilitators to Auditors of Implementation Quality. However, this auditing is governed by a fundamental architectural constraint:
- Zero-Visibility (Blind-to-Transit): The NHA has no visibility into health data while it is in transit or at rest. They only provide the discovery and consent layer. This is a deliberate privacy-first design choice.
- Fiduciary Responsibility: Because the NHA cannot "see" the data, the Hospital (the fiduciary) remains solely responsible for any missing, inaccurate, or incomplete documentation. The responsibility for data presence and integrity stays at the clinical source.
- Quality Auditing: NHA's role is to ensure that the software implementers provide the capability for structured data, but the onus of population and accuracy remains with the originating institution.
DPDP Act and the Right to Forget: Consent Governance
The newly enacted Digital Personal Data Protection (DPDP) Act introduces a fundamental shift in patient agency:
- Consent Autonomy: Consent is now recognized as a non-negotiable right. A patient can withdraw consent at any point in time, effectively opting out of the discovery layer for specific longitudinal records.
- The Medico-legal Dilemma: This autonomy raises complex questions for medico-legal cases. If a patient withdraws consent for a record that is critical to an ongoing legal proceeding, the ecosystem must navigate the friction between individual privacy rights and the judicial requirement for evidence.
- Patient Awareness & Empowerment: The current focus of the mission is shifting toward large-scale Patient Education. The goal is an ecosystem where every citizen understands their rights under the DPDP Act and the benefits of maintaining a secure, linked health history.
The Implementation Frontier: HIE & Operational Realities
Bridging the gap between a "digital vision" and "operational reality" requires addressing the technical and governance frictions of a national Health Information Exchange (HIE).
The Standards Paradox (HL7 v3 vs v2.7)
Interoperability is often hampered by Versioning Conflict. While national missions advocate for modern standards (FHIR), most legacy hospital systems (LIS/RIS) still run on HL7 v2.x. - Data Integrity Risk: Forcing a match between HL7 v3 (XML) and HL7 v2.7 (Pipe-delimited) can lead to "semantic slippage," where critical clinical flags or lab nuances are lost during translation. - The Middleware Requirement: Successful HIE implementation requires robust Intermediate Mapping Layers that can handle these versioning mismatches without data loss.
OPD Success vs. The CDA Challenge
India has seen massive success in digitizing Out-patient (OPD) registration and summaries. However, the next frontier is the Clinical Document Architecture (CDA): - OPD (Snapshot): Success is driven by simple, structured summaries. - Inpatient (Narrative): Complex inpatient care requires a more robust CDA/CCR (Continuity of Care Record) framework to capture the longitudinal depth of a patient's stay, which remains a significant implementation hurdle for most hospitals.
Data Ownership vs. Digital Lockers
A common governance misunderstanding involves the "ownership" of medical data: - Ownership: The Hospital (the fiduciary) remains the owner and custodian of the primary clinical record. - The Locker (Locker/PHR): Platforms like the ABDM Health Locker are not owners; they are secure gateways designed to provide the patient with agency over their own health history.
International Benchmarking
India's federated approach draws parallels with global leaders, yet remains unique:
The Federated Edge: India's Unique Architecture
Unlike centralized models, India's HIE is designed as a Federated Architecture, ensuring that data stays at the source while allowing discovery and consent-based access at a national scale.
Advanced Implementation Insights: Agency, Scale, and Friction
The evolution of India's digital health mission is uncovering deep technical and regulatory insights into how scale and agency are truly achieved.
Patient Agency: The PHR Link Model
A core tenet of the ABHA ecosystem is empowering the patient as the primary orchestrator of their medical history. - The Push Mechanism: Instead of a central repository, the system uses a Link and Share model. Patients receive a digital link (via PHR apps like the ABHA app) to their clinical records for both Out-patient (OPD) and In-patient (IPD) care. - Longitudinal History: By linking these fragmented visits, the patient maintains a continuous, longitudinal health record that they can share with any clinical provider, regardless of the hospital's internal HIS.
Population Health & The ABHA Aggregate
Beyond individual care, the digitization of clinical records opens the door to massive Population-wide Health Insights. - Aggregated Data for Trends: The federated architecture allows for the collection of anonymized, aggregated data to track disease outbreaks, treatment efficacy, and public health trends at a national level. - Research Partnerships: This data serves as a critical asset for academic and clinical research, enabling partnerships between the NHA, research institutions, and the private sector to drive evidence-based medicine.
Data Without Borders: International Portability
The technical standards adopted by India (FHIR, SNOMED CT) are designed with International Interoperability in mind. - Cross-Border Continuity: The next frontier is enabling the portability of health records for Indian citizens traveling or living abroad, ensuring that their medical history is accessible and semantically understood by global healthcare systems. - Global Standards Alignment: By adhering to international norms, India ensures that its digital health infrastructure is compatible with emerging global health data exchange frameworks.
The Private Sector Paradox: Regulatory & Operational Friction
While the government sector has shown aggressive adoption, the private sector faces unique Implementation Frictions. - Licensing & Compliance (DMHO): Private hospitals often navigate a complex regulatory landscape, where digital adoption is linked to DMHO Licensing and other state-level compliance "sticks." - The Mandate Gap: Unlike government-led institutions, private hospitals must balance the high cost of digital transformation with operational profitability, often leading to a slower adoption curve unless mandated by national insurance schemes or regulatory requirements. - Strategic Concentrate: As a result, the most robust "advanced" implementations are currently concentrated in large public sector institutions, creating a "digital maturity gap" that the next phase of the mission aims to close.
Data Architecture: Managing Volume, Velocity, and Variety
The digital health ecosystem is characterized by an explosion of Heterogeneous Data. As clinical services expand from in-patient tracking to remote monitoring and intelligent diagnostics, the technical architecture must evolve to handle the increasing Volume and Velocity of data flows.
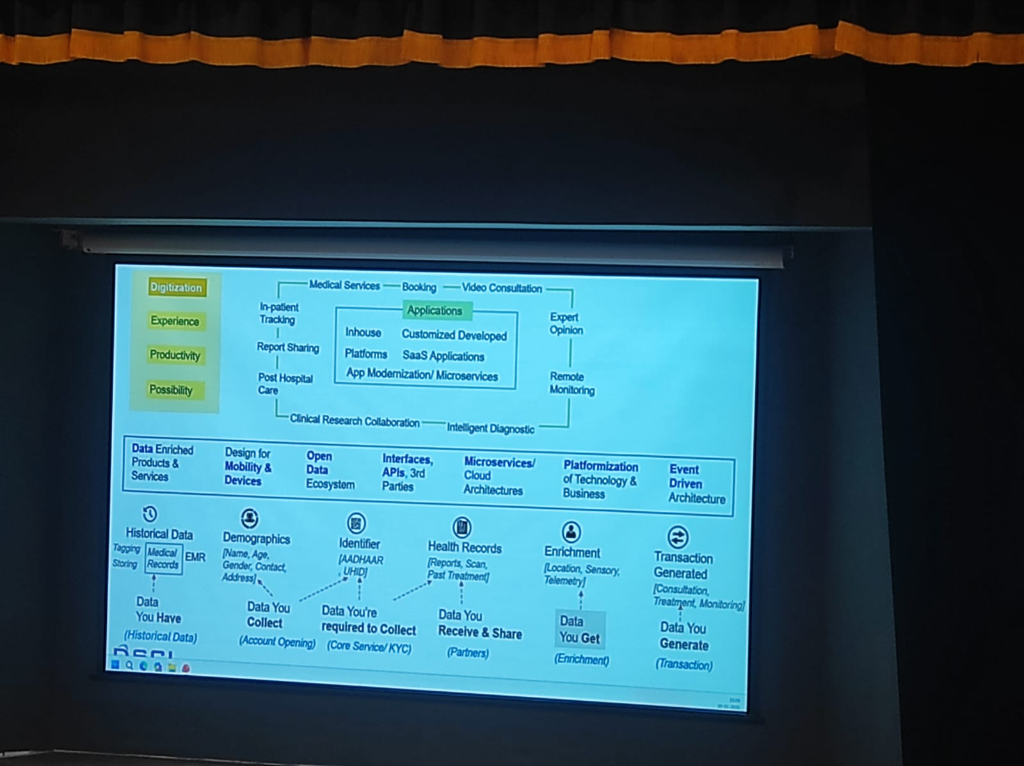 Figure: The 6-step clinical data journey—from historical records to transaction-generated insights.
Figure: The 6-step clinical data journey—from historical records to transaction-generated insights.
Successful digital health platforms manage data through a structured lifecycle, as demonstrated in the national framework:
- Historical Data (What you Have): Digitizing legacy medical records and EMR tagging.
- Demographics (What you Collect): Initial account opening and patient identification.
- Identifier (What you're Required to Collect): Anchoring the patient to national standards (ABHA/UHID).
- Health Records (What you Receive & Share): Interoperable exchange of clinical reports and scans with partners.
- Enrichment (What you Get): Adding sensory, telemetry, and location data to the patient profile.
- Transaction Generated (What you Generate): The final clinical outcome—consultations, treatments, and continuous monitoring.
App Modernization & Microservices
To prevent architecture stagnation, hospitals are shifting toward App Modernization. This involves moving from rigid, monolithic HIS systems to Microservices and SaaS-based cloud architectures. This modularity is essential for scaling Intelligent Diagnostics and facilitating Clinical Research Collaboration across institutions.
The Spectrum of Healthcare Data
Before diving into infrastructure, it is vital to understand the diversity of data that flows through a digital health ecosystem. Medical data is not just an EMR; it is a complex mosaic of diverse identifiers and sources, influenced heavily by Who is being monitored and How the components integrate.
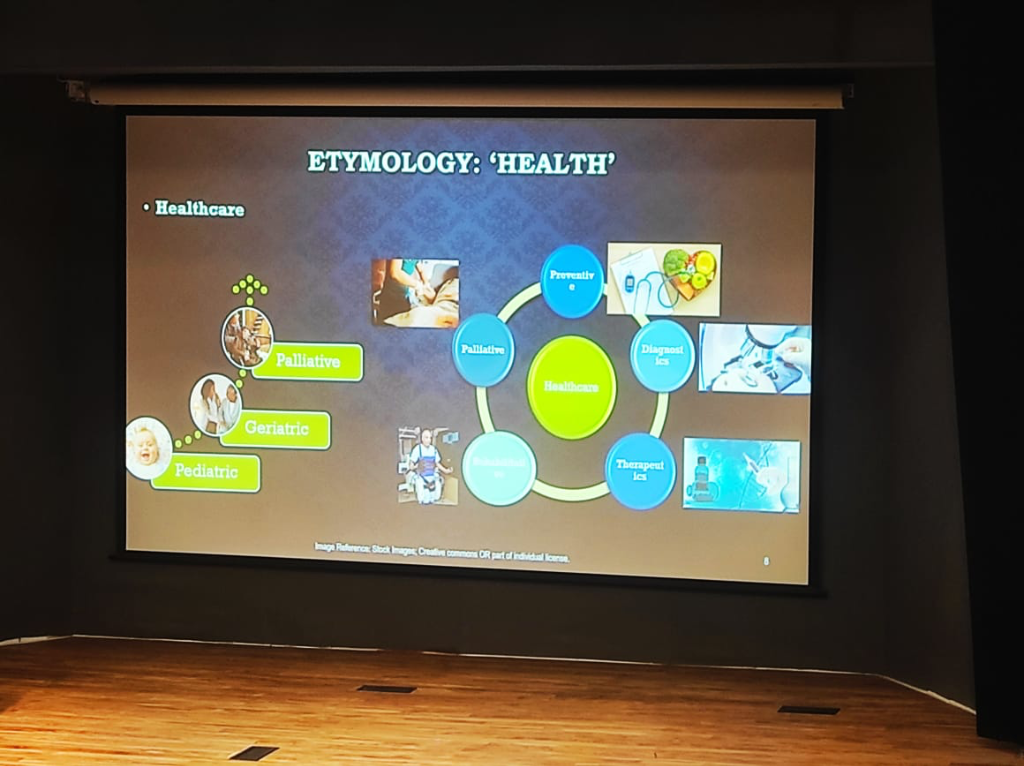 Figure: The holistic landscape of healthcare—integrating Preventive, Diagnostic, Therapeutic, and Palliative care across diverse patient cohorts from Pediatric to Geriatric.
Figure: The holistic landscape of healthcare—integrating Preventive, Diagnostic, Therapeutic, and Palliative care across diverse patient cohorts from Pediatric to Geriatric.
The System Dilemma: Cohorts & Complexity
Any digital health strategy must account for two critical variables that define its clinical and technical success:
- Cohort-Specific Significance: The clinical relevance of data is not absolute; it is relative to the patient population. Clinical baselines and urgency thresholds shift dramatically across the life-cycle—from Pediatric to Geriatric and eventually Palliative care. A data point that is merely "noise" in one group may be a "critical signal" in another.
- The Debugging Paradox: In health tech, "debugging" is rarely about fixing a single broken component. Individual parts—a wearable sensor, a cloud API, or an EHR database—often function perfectly in isolation. The real challenge emerges when these Individual Components Come Together. Addressing problems in such a system requires a "systems-thinking" approach to identify failures at the integration points rather than within the components themselves.
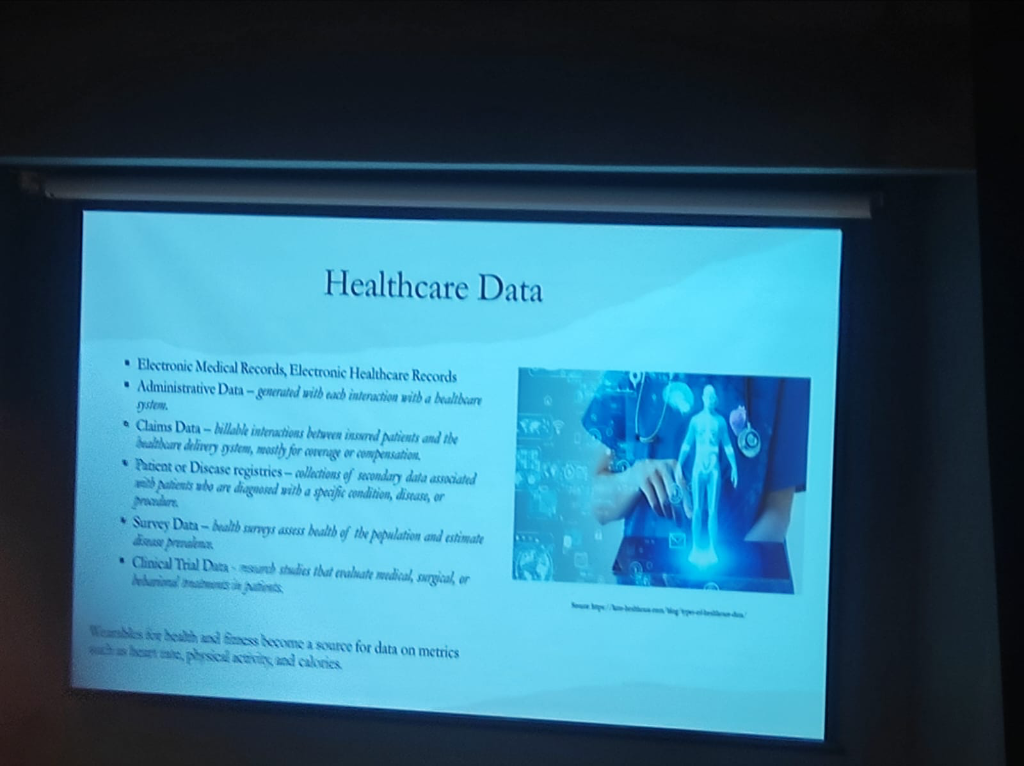 Figure: The diverse landscape of healthcare data—from clinical EMRs and administrative records to billable claims, disease registries, health surveys, and wearable-generated metrics.
Figure: The diverse landscape of healthcare data—from clinical EMRs and administrative records to billable claims, disease registries, health surveys, and wearable-generated metrics.
- Electronic Medical & Health Records (EMR/EHR): The core clinical longitudinal record.
- Administrative Data: Generated with every system interaction (registrations, scheduling, bed management).
- Claims Data: Billable interactions between insured patients and the healthcare delivery system, primarily for coverage and compensation.
- Patient or Disease Registries: Secondary data associated with patients diagnosed with specific conditions (e.g., Oncology or Cardiac registries).
- Survey Data: Health surveys that assess the health of the population and estimate disease prevalence.
- Clinical Trial Data: Research studies that evaluate medical, surgical, or behavioral treatments in patients.
- Wearable & Fitness Data: A growing source of continuous metrics such as heart rate, physical activity, and calories. Consumer ecosystems like Apple Health are now collecting more data than most patients realize, making institutional governance of this stream increasingly critical.
The Continuous Monitoring Revolution: Primary vs. Derived Data
The integration of wearables marks a shift from periodic snapshots to Continuous Scanning. However, a foundational principle must guide this integration: Medical-grade wearables and consumer-grade devices are not the same.
While consumer ecosystems like Apple Health are prolific, they primarily offer Surrogate or Derived Data, which must be distinguished from Primary Clinical Data:
- Primary Data: Direct, raw clinical measurements or waveforms (e.g., a chest ECG patch providing raw electrical activity).
- Derived & Surrogate Data: Algorithmic outputs that proxy clinical states. For instance, HRV, Heart Rate, and Respiratory Rate on consumer smartwatches are often derived via PPG (photoplethysmogram) sensors and proprietary algorithms.
- The Informed Second Opinion: Managed effectively, these provide a valuable "informed second opinion" for pre-clinical tracking and medication titration, but they carry inherent technical risks:
- False Positives & Alarm Fatigue: Consumer-grade ecosystems (Apple, Garmin, Smart Rings, and even consumer Chest Straps) frequently generate false positives. Without clinical-grade filtering, these signals can lead to unnecessary patient anxiety and clinician "alarm fatigue."
- Technical Artifacts: Motion artifacts can significantly distort readings from consumer-grade trackers during daily activity.
- Biochemical Dependencies: Precision varies by technology. For example, Continuous Glucose Monitors (CGMs) use enzymatic reactions (glucose oxidase) that are sensitive to underlying oxygen level fluctuations or respiratory disorders.
- Algorithmic Opacity: Unlike clinical-grade equipment, consumer devices often lack transparent algorithmic validation for their derived parameters.
- Snapshot vs. Continuous Monitoring: A critical void exists in measurement duration and continuity. An Apple Watch ECG, for instance, is an on-demand 30-second snapshot—functionally different from hospital-grade continuous telemetry.
- The CGM "Closed-Loop" Gap: While CGM patches provide more frequent data, they are limited by wearable duration (sensor drift after 10-14 days) and, critically, a lack of Closed-Loop integration. In consumer-grade tech, the data is often "monitoring-only," lacking the integrated therapeutic response required for clinical management.
Wearable Intelligence: Extracting Signal from Noise
The true "intelligence" of a wearable does not reside in the hardware module but in the Algorithm. This is especially critical because Raw Data is Junk from a clinical perspective, particularly when the user is active.
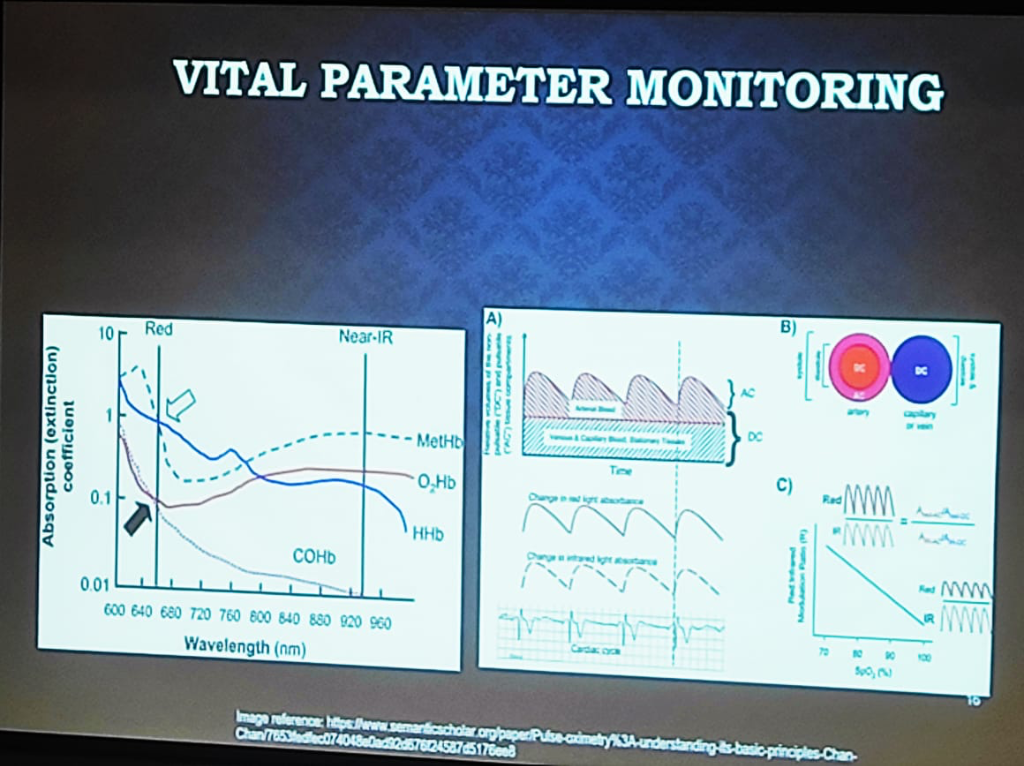 Figure: The physics of Vital Parameter Monitoring—showing the absorption (extinction) coefficients of hemoglobin states and the separation of pulsatile (AC) and stationary (DC) signal components.
Figure: The physics of Vital Parameter Monitoring—showing the absorption (extinction) coefficients of hemoglobin states and the separation of pulsatile (AC) and stationary (DC) signal components.
- The Pulse Oximetry (PPG) Spectrum:
- Medical-Grade: Uses a combination of Red and NIR (Near-Infrared) wavelengths. It relies on the ratio of the pulsatile (AC) part to the stationary (DC) part of the signal across both wavelengths to calculate oxygen saturation accurately.
- Consumer-Grade: Often uses Green Wavelengths (providing maximum reflectance) for heart rate tracking. While these devices handle Single-Point (Snapshot) measurements reasonably well, maintaining clinical significance and signal integrity Over Time (Longitudinal) is a significantly greater engineering hurdle. Baseline drift, changing sensor-to-skin contact, and environmental fluctuations make consistent long-term monitoring with consumer hardware a complex algorithmic challenge.
- Mechanical Interference (The "Tight Wear" Problem): Signal integrity is sensitive to physical application. A common clinical error in consumer wearables is excessive wearing pressure. Wearing a smartwatch or ring too tightly can compress the underlying capillaries and venous structure, distorting the pulsatile (AC) components and altering the stationary (DC) baseline. This mechanical interference leads to incorrect parameter extraction, as the algorithms cannot distinguish between physiological pulse and pressure-induced artifacts.
- Environmental & Chemical Dependencies: precision varies by the underlying technology and ambient conditions:
- Trend over Truth (Absolute Value Inaccuracy): A critical clinical caveat for Continuous Glucose Monitors (CGMs) is the inherent inaccuracy of Absolute Values. Most consumer and intermediate-grade CGMs are not designed for the same level of spot-check precision as clinical finger-prick glucometers. However, in clinical practice, the Trend and Range (Time-in-Range) provided by the CGM is more than enough for effective monitoring and behavioral intervention. The clinical utility lies in revealing longitudinal patterns and glycemic variability over time, rather than absolute precision at any single moment.
- Biochemical & Non-Invasive CGMs: Traditional monitors use enzymatic reactions (glucose oxidase) sensitive to oxygen levels. However, next-generation Non-Invasive Glucose Monitoring (e.g., smart rings or PPG-based patches) faces two massive engineering hurdles:
- The Water Interference Problem: Glucose has specific absorption peaks (e.g., 850nm, 950nm, 1150nm), but these often overlap with water content peaks. Since the human body is primarily water, extracting the "glucose signal" from the "water noise" is a significant technical challenge.
- The Calibration Void: There is no universal calibration curve for non-invasive sensing. Individual physiological variability (Skin Type, Body Type, Hydration) means that "Person A" and "Person B" will have completely different absorption characteristic curves for the same glucose level. Accuracy requires combining raw PPG data with patient-specific parameters via an AI Intelligence Layer to create personalized calibration models.
- Humidity vs. Mechanical Strain: Respiratory monitoring reveals a critical technical divide. Chest Straps measure lung expansion via mechanical strain, while newer mask-integrated sensors (as shown below) may rely on Humidity Levels and airflow. Environmental factors like ambient humidity can create significant discrepancies between these modalities when measuring lung capacity, requiring complex compensation algorithms to ensure clinical accuracy.
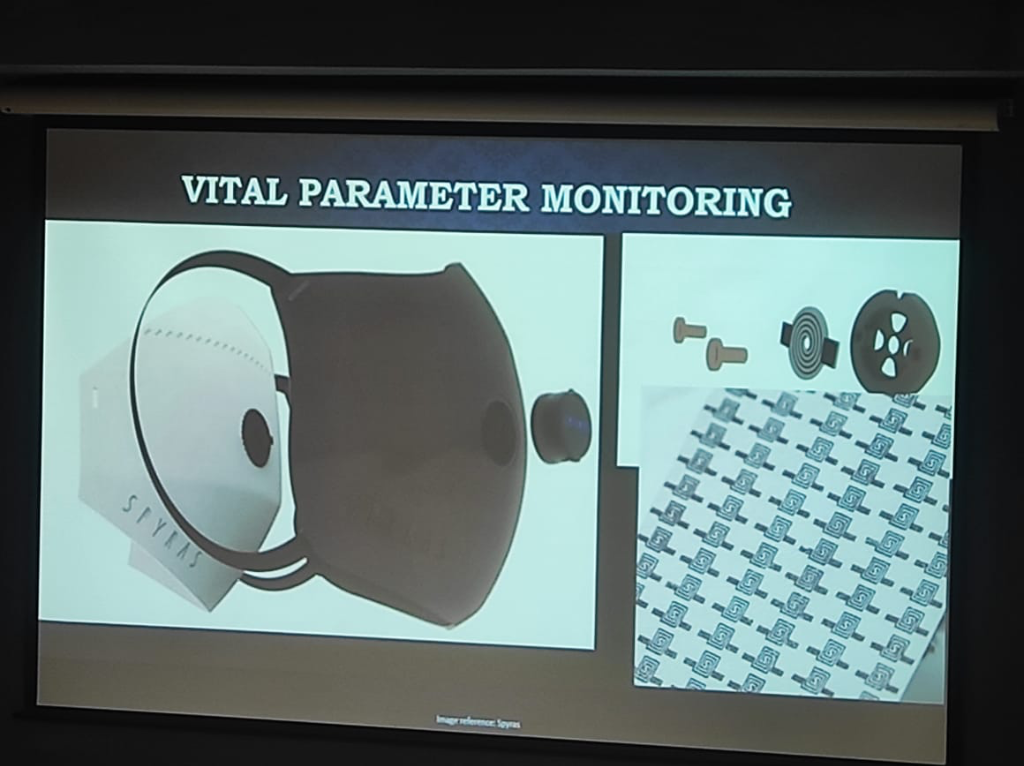 Figure: Advanced Respiratory Monitoring—demonstrating the integration of sensors into masks to capture vital parameters via airflow and humidity, moving beyond simple mechanical chest straps.
Figure: Advanced Respiratory Monitoring—demonstrating the integration of sensors into masks to capture vital parameters via airflow and humidity, moving beyond simple mechanical chest straps.
- The Multi-Factor Noise Landscape: Beyond motion, PPG signal integrity is threatened by a spectrum of environmental and mechanical noise sources that engineering teams must address through Device Geometry and signal processing:
- Environmental Optical Noise: Sensors must differentiate between the pulsatile clinical signal and ambient stray light. This requires complex compensation for background lighting to prevent signal saturation.
- Electromagnetic Interference (EMI): Power line noise and interference (PLI) can introduce electrical artifacts that mimic physiological rhythms.
- Temperature & Sensor Performance: Thermal variations can affect sensor sensitivity, electrode-to-skin contact, and the performance of medical adhesives, creating a shifting baseline for data extraction.
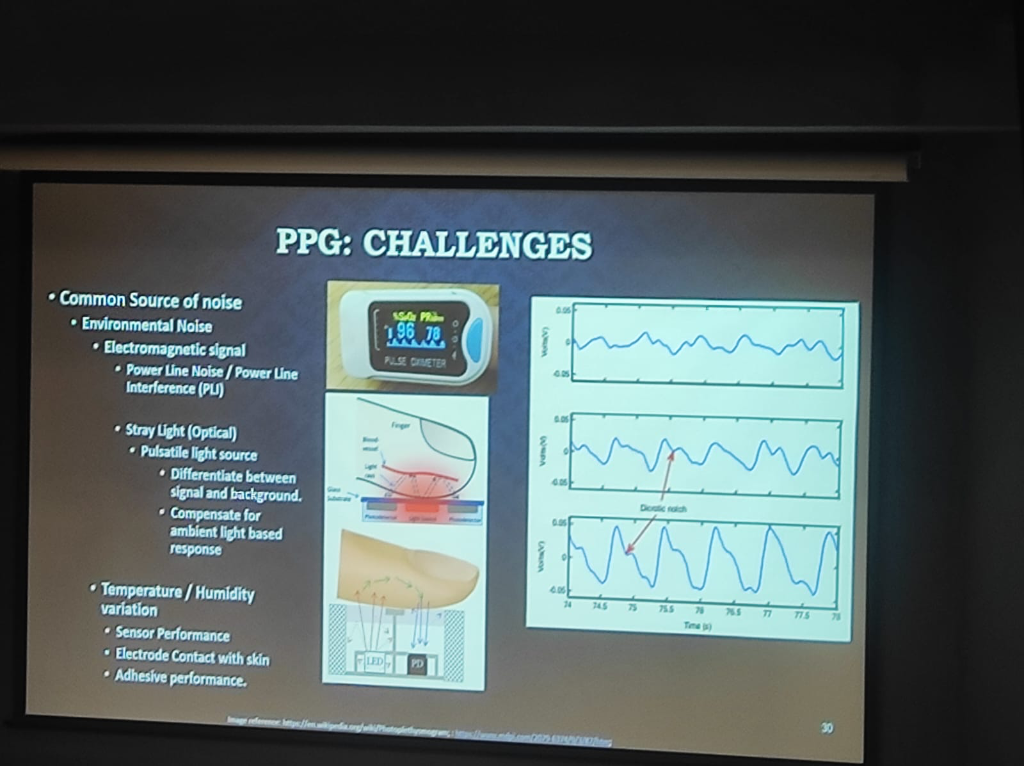 Figure: The spectrum of PPG Challenges—detailing environmental noise (EMI, Stray Light) and the impact of temperature/humidity on sensor and electrode performance.
Figure: The spectrum of PPG Challenges—detailing environmental noise (EMI, Stray Light) and the impact of temperature/humidity on sensor and electrode performance.
Engineering Actionable Data: Beyond the API
Creating an actionable EHR from wearable data requires solving five critical engineering and clinical challenges:
- The Semantic Gap (Algorithm Variance): Identical units (e.g., milliseconds) do not guarantee identical meaning. For instance, Heart Rate Variability (HRV) can be calculated via different formulas—Standard Deviation of NN intervals (SDNN) vs. Root Mean Square of Successive Differences (RMSSD). Different devices (Apple, Garmin, Fitbit) generate proprietary "Sleep Scores" or "Stress Scores" that are not semantically comparable. Bridging this gap requires mapping diverse algorithmic outputs to a unified clinical standard.
- The Temporal Gap (Continuance vs. Episodic): Modern EHRs are fundamentally built for Episodic Data—capturing distinct clinical events (visits, labs, surgeries). In contrast, wearables generate a Continuous High-Frequency Stream. Injecting raw continuous data into an episodic HIS causes "storage bloat" and clinician data-overload. System architects must implement "intermediate refinement" layers that convert continuous streams into meaningful episodic summaries or "parameter reports" (as seen in CGM reports) before EHR injection.
- Activity-Aware Normalization: Raw data is meaningless without context. Normalization must be "activity-aware" to create valid Optimal Baselines. Heart rate during sleep vs. heart rate during a marathon are two different data points; without normalization, they cannot be used to detect clinical anomalies.
- Contact Verification: Physiological significance relies on signal quality. Modern clinical governance must include algorithms to verify appropriate body contact, ensuring the device hasn't slipped or lost its sensor-to-skin integrity.
- Clinical Workflow Integration: The final metric of success for wearable data is not technical accuracy, but its impact on the clinical workflow. Global precedents, such as Mayo Clinic's integration of Apple Watch data and Western institutional CGM-based studies, demonstrate that integration must prioritize Burden Reduction for clinicians:
- Event-Based vs. Continuous Flow: Systems should move away from dumping continuous raw datasets. Instead, integration should be Event-Based—where specific algorithmic triggers (e.g., a detection of sustained tachycardia or oxygen desaturation) inject data into the EHR only when clinical attention is warranted.
- Longitudinal Trend Summaries: Clinicians need the ability to view deterioration over time. Rather than relying on proprietary manufacturer scores (which are often "black boxes"), institutions should define their own Clinical Indices for trend-based analysis.
- The Actionable Loop (Medication Continuity): Successful models involve Weekly Summaries where data trends are reviewed to provide active clinical recommendations. This includes adjustments for Medication Continuity, ensuring that wearable data isn't just monitored but used to close the therapeutic loop.
- Data Parsimony & Clinical Intent: We must question the volume of data collected based on clinical objectives. For instance, CGM monitoring for a patient not at risk of hypoglycemia may only require a 14-day trend to capture intermediate glycemic variability—after which the utility of continuous data plateau. Conversely, Cardiac monitoring requires long-term longitudinality and high-resolution indices. In clinical practice, Indices are more important than raw data volume.
- Human-in-the-Loop Escalation: Actionable data must be embedded within an escalation logic. This includes sharing data to ICU-style workstations with clear escalation paths and maintaining a "Human-in-the-Loop" for final therapeutic decisions.
- The Practical Delivery Gap (Email/WhatsApp vs. EHR): A major hurdle in the current landscape is the delivery modality. Most CGM data reports are currently shared via Email or WhatsApp rather than being natively integrated into a professional EHR. This creates a fragmentation gap where vital wearable insights exist as loose attachments or messages rather than being part of a structured, longitudinal clinical history. True integration requires moving these reports from consumer apps into the core clinical information system.
- Proximity vs. Significance: A foundational clinical principle is that physical proximity does not correlate to physiological significance. A recent example is the Zomato CEO wearing a CGM (Continuous Glucose Monitor); while the device was physically attached and generating data, its physiological significance is limited when used by a healthy individual without clinical indication. Data without clinical intent is merely noise, not medicine.
The Data Lifecycle: A Governance Framework
Managing this diverse data requires a structured lifecycle approach. As hospitals transition to "Privacy-First" architectures, the process of how data is collected, used, and shared becomes more important than the simple act of storage.
 Figure: The 5-stage Data Lifecycle—Capture, Process, Use, Store, and Dispose—providing the foundational timeline for clinical data governance.
Figure: The 5-stage Data Lifecycle—Capture, Process, Use, Store, and Dispose—providing the foundational timeline for clinical data governance.
- Capture: Securely ingest data into health information systems from clinical, administrative, or wearable sources.
- Process: A series of automated and manual actions taken to create and offer clinical products and health services.
- Use: The critical phase of Access, Sharing, and Analysis. This is the most important process for most modern systems, where governance must be strictly enforced.
- Store: Maintaining and archiving data in encrypted, high-availability environments.
- Dispose: The often-neglected final step—ensuring secure destruction per retention schedules to limit long-term liability.
At every stage of this lifecycle, hospitals must adopt the principle of Data Minimization:
- Lower Costs: Collecting only what is necessary reduces the massive storage and processing overhead on clinical infrastructure.
- Reduced Risk: Minimizing the data footprint directly lowers the surface area for potential breaches and DPDP liability.
- Privacy by Default: Moving from "collect everything" to "collect what is required" is the cornerstone of a modern, compliant health system.
Infrastructure Essentials: The "Hardware Blind Spot"
A critical gap in digital health transformation is the clinician's awareness of the underlying physical infrastructure. Successful implementation requires understanding the Bill of Materials (BOM) and the foundational requirements for operational stability.
The maturity of a hospital's digital infrastructure is often determined by its location. The City Classification (Tier 1 vs. Tier 2/3) dictates the "Class of Hardware" available and the feasibility of cloud-native deployments:
- Tier 1 Cities: High bandwidth availability and reliable power make Cloud-Native architectures and advanced hardware deployments more feasible.
- Tier 2/3 Cities: Internet instability often mandates a Heavily On-Premise or hybrid approach, with specialized ruggedized hardware to handle environmental stressors.
For a hospital to function digitally, the infrastructure must be treated with the same rigor as surgical equipment:
- Networking as a Priority: Enterprise-grade networking is the most underestimated cost. High-performance managed switches and robust structured cabling (Cat6/Fiber) are essential to prevent the "system is slow" bottleneck.
- The Power Factor: Redundant power supplies and industrial-grade UPS systems are non-negotiable for 24/7 clinical continuity.
- Terminal Devices: A mix of specialized medical-grade tablets, bedside terminals, and high-resolution diagnostic monitors.
Mission-Critical Design: "Running with Hands Tied"
In many clinical settings, direct internet access is prohibited for security reasons. Designing for these "air-gapped" or restricted environments requires a shift in engineering philosophy toward high availability and resilience.
Hospital Network Topology
For a 500-bed hospital, the network must be tiered to ensure that a failure in one ward doesn't paralyze the entire institution:
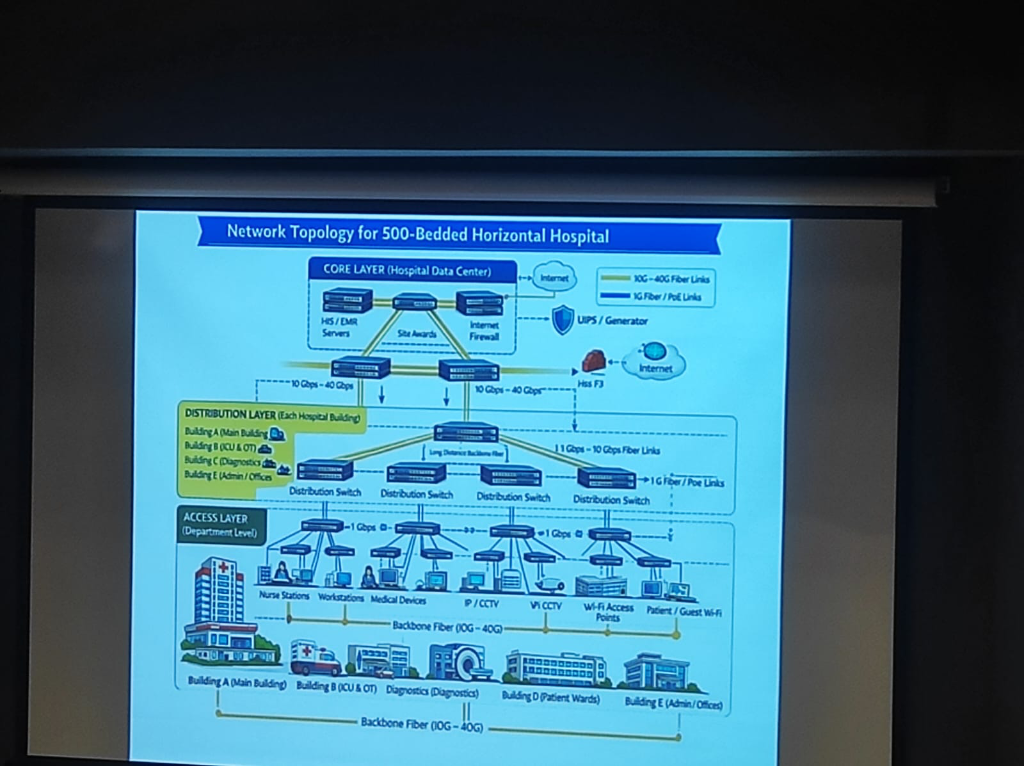 Figure: A formal 3-layer topology (Core, Distribution, Access) designed for zero-downtime clinical operations.
Figure: A formal 3-layer topology (Core, Distribution, Access) designed for zero-downtime clinical operations.
- Advanced Availability Architecture: Hospitals must eliminate single points of failure through a robust technology stack:
- High Availability (HA) & Clustering: Grouping servers into clusters to ensure that if one node fails, another takes over instantly without service interruption.
- Data Replication: Real-time mirroring of clinical databases across multiple storage engines to prevent data loss.
- Failover & Disaster Recovery (DR): Automated failover mechanisms to a secondary Disaster Recovery site (on-prem or cloud backup) ensuring continuity during catastrophic failures.
- Zero-Downtime Resilience: Hospitals cannot afford a "wait period." Systems must be designed for Triple Redundancy (Local, On-Prem Backup, and DR site) to ensure clinical continuity 24/7.
- PAC Systems & High Throughput: Medical imaging (PACS) generates massive data volumes. This requires High-Throughput Storage and dedicated high-speed VLANs to ensure radiologists and surgeons can access 3D scans instantly without network lag.
- Scalability for Expansion: Infrastructure must be modular, allowing for "plug-and-play" expansion of departments without overhauling the core network backbone.
Privacy: An Ethical & Fiduciary Foundation
The push for digital health privacy is not merely a legal requirement; it is rooted in centuries of Medical Ethics and the unique nature of the clinical bond. Within this framework, Data Security is the means to achieve Privacy Rights—the technical foundation that makes individual agency possible.
Respect for Autonomy
A fundamental principle of medical ethics is the Respect for Autonomy. This gives patients the right to ensure that data pertaining to them is not accessed by anyone unless it is absolutely necessary for the specific service being provided. Privacy is the mechanism through which this autonomy is exercised in a digital system.
The doctor-patient relationship is fundamentally a Fiduciary Relationship—a bond built on trust, reciprocity, and an implicit promise of safety:
- Trust & Reciprocity: Patients share their most sensitive information with the faith that it will be used only for their benefit. In return, doctors rely on the truthfulness of that information to provide accurate care.
- The Confidence Mandate: Clinical interaction requires a level of confidentiality that prevents harm to the patient. Without explicit assurance from the healthcare ecosystem, patients will not willingly part with their sensitive health data.
DPDP: Substantiating Medical Values
The Digital Personal Data Protection (DPDP) Act, 2023 should not be viewed as "reinventing the wheel." Instead, it is a regulatory framework that substantiates existing medical ethics with a better, more robust legal structure. It codifies the principles of confidentiality and no-harm that have always been the bedrock of healthcare.
Security & Compliance: The Global Mandate
The AIIMS hacking case serves as a stark reminder that simple firewalls are no longer enough. Security must be multi-layered, compliant with global standards, and rooted in the principle of Security by Design—where protection is an architectural requirement, not an afterthought. Governance now mandates a "Privacy-First" approach to how data is collected, processed, and shared.
Medical data is a global asset requiring adherence to rigorous regulatory frameworks:
- NABH (India): National Accreditation Board for Hospitals & Healthcare Providers standards for operational and data quality, now featuring a progressive maturity framework for digital health.
- HIPAA (USA): While often perceived as the healthcare "gold standard," HIPAA compliance does not automatically satisfy local DPDP mandates. Indian hospitals must cater to specific local nuances and rights not covered by US legislation.
- GDPR (EU): The General Data Protection Regulation, providing stringent privacy requirements that served as a partial model for the DPDP Act.
- DPDP Act 2023 (India): The definitive, compulsory national legislation for data handling in India, mandating strict consent and introducing unique rights and heavy penalty liabilities. The rules are expected to be fully enacted by April 2026.
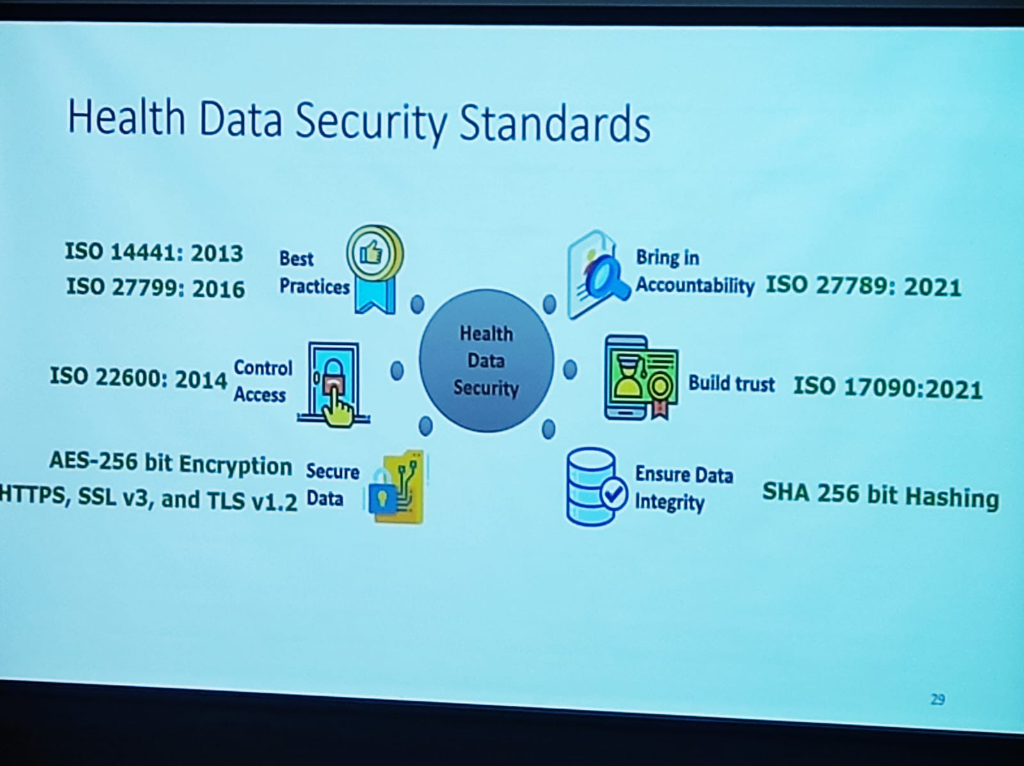
Security is not just a policy; it is built on a foundation of rigorous international standards that ensure Resilience and Trust:
- Robust Frameworks: Adherence to ISO 27001, 14441, 27799, 22600, 27789, and 17090 provides the global benchmark for health data security.
- Technical Safeguards: Implementing AES-256 bit Encryption for data on the wire and SHA-256 bit Hashing to ensure data integrity.
- Granular Security Policies: True security extends to human behavior. Institutions must enforce policies for Remote Work (secure protocols) and Clear Desk & Clear Screen (mandatory system locking) to prevent accidental data exposure.
- Operational Disruption: The DPDP Act is a workflow disruptor. Since every discrete data point in a hospital involves personal health information, compliance impacts every aspect of management—from front-desk registration to clinical discharge.
Beyond national legislation, clinical data governance is bolstered by a network of sectoral policies and ethical guidelines:
- IMC Regulations 2002: Directs the maintenance of medical records for specific retention timelines and mandates the computerization of records for quick and accurate retrieval.
- National Ethical Guidelines (Human Research): Establishes policies for data capture, acquisition, sharing, and ownership, emphasizing the role of Ethics Committees in safeguarding participant privacy.
- ART Act 2021: Specifically mandates that assisted reproductive technology clinics and banks protect all confidential information and maintain accurate, secure records.
- ICMR Lab Guidelines 2021: Defines rigorous standards for Good Clinical Laboratory Practices, focusing on multi-dimensional security (Hardware, Network, Application, Personnel) and mandatory Disaster Recovery planning.
A critical nuance in Indian digital health governance is the relationship between the Ayushman Bharat Digital Mission (ABDM) and the DPDP Act:
- Voluntary vs. Compulsory: While ABDM participation is a voluntary framework for hospitals, the DPDP Act is a compulsory, legislative mandate.
- The HDMP Trigger: Once a hospital volunteers for the ABDM ecosystem, it automatically triggers the Health Data Management Policy (HDMP)—a sectoral regulation that mandates:
- Secure Storage: Ensuring digital health records are stored in encrypted, compliant environments.
- Rigorous Access Controls: Enforcing role-based access for every clinical interaction.
- Breach Reporting: Mandatory reporting systems for any security incident within the ABDM network.
- ABDM-Certified Tools: Hospitals are increasingly mandated to rely on ABDM-certified tools (EMRs, LIMS, Health Lockers) that have been vetted for these sectoral security standards.
Regulatory Risk: The "Dual Penalty" Threat
Non-compliance in a digitized environment carries a double-edged risk. A data breach doesn't just trigger one investigation; it triggers two: 1. Sectoral Penalty: Penalties and blacklisting under the ABDM/National Health Authority (NHA) framework for violating the Health Data Management Policy. 2. National Penalty: Massive financial penalties (up to ₹250 Crores) under the DPDP Act 2023 for failure to protect personal data. This dual-track liability makes investment in robust cybersecurity not just an IT goal, but a core strategy for institutional survival.
The implementation of the Digital Personal Data Protection (DPDP) Act, 2023 represents a monumental shift for Indian healthcare. As Bagmishka Puhan (Associate Partner, TMT & Digital Health Legal) details, privacy is no longer an option; it is a Fundamental Right.
The High Stakes of Compliance The Act introduces a regime of Heavy Penalties specifically targeting Breach Liability. Hospitals must now navigate substantial procedural norms, from Breach Reporting and Grievance Redressal to maintaining a robust Regulatory Architecture.
Core Challenges for Hospitals:
- Personal Data & Scanned Documents: Under DPDP, "Personal Data" is any identifier that can pinpoint an individual, either by itself or in conjunction with other data sets. Crucially, the Act applies to data collected in digital form or collected in non-digital form and digitized subsequently (the "Scanned Document" rule).
- Unique Indian Rights: The Act introduces rights that do not exist in traditional global legislation (like HIPAA or GDPR), requiring institutions to build specific technical interfaces for:
- Right to Nominate: The ability for a patient to nominate a person who will exercise their rights in case of their disability or death.
- Right to Grievance Redressal: A mandatory, institutionalized mechanism for addressing user complaints.
The Patient's Charter: Rights of the Data Principal
Under the DPDP Act, patients (Data Principals) are granted a comprehensive charter of rights designed to restore their agency over their health data:
- Right to Access & Control: Patients can request information about their personal data and obtain a summary of data processed.
- Right to Correction & Erasure: The right to update inaccurate data and request the deletion of data once the purpose is served.
- Right to be Informed: Beyond just data, patients have the right to be given information about tests, treatment options, and their associated benefits and risks.
- Right to Informed Choice: The mandate to make an informed choice and provide explicit Informed Consent before processing begins.
- Right to Safety & Security: The right to expect providers to keep health information safe and secure at all times.
- Unique Indian Mandates: The Right to Nominate (for disability or death) and the Right to seek treatment from a registered medical practitioner (noting the mandatory requirement of identification).
- Applicability & Directions: Understanding the specific legal directions for various healthcare departments.
- Quantum & Complexity: Managing the massive volume and diversity of health data under strict procedural obligations.
- Due Diligence & Compliance Demonstration: The burden of proof is on the institution—hospitals must proactively demonstrate they have secured patient data.
Data Protection: Clinical Best Practices
Implementing a resilient privacy framework requires moving from policy to practice. The following 8-pillar framework defines the gold standard for clinical data protection:
- Strict Data Minimization: Collect and process only as much data as is strictly necessary for the therapeutic purpose.
- Recorded Consent: Ensure that every piece of patient data is backed by recorded, unbundled consent.
- Need-to-Know Access: Restrict access to patient files only to users who have a legitimate clinical or administrative requirement.
- Lifecycle Security: Ensure data is secure at all points of interaction—from capture to archive.
- User-Driven Accuracy: Allow patients to update or verify their information, ensuring clinical record integrity.
- Statutory Retention: Retain data only as long as required by law or for the legitimate purpose for which it was collected.
- Timely Deletion: Permanently delete personal data when there is no further clinical or legal need for its retention.
- Accountability & Auditing: Maintain logs and conduct regular audits to ensure the entire lifecycle of the data is accounted for.
- Annual Governance Audits: Conduct a mandatory annual audit specifically targeting Data Deletion, Retention policies, and Purging schedules to ensure technical execution matches clinical and legal mandates.
The Transformation Path (Response Strategy): To survive this regulatory shift, institutions must move from simple awareness to active participation:
- Comprehensive Contextualization: Mapping DPDP principles to specific clinical workflows.
- From Commitment to Ownership: Shifting accountability from a single "IT person" to clinical and quality leads.
- From Ethics to Compliance Culture: Building a moral consensus across the hospital that prioritizes Privacy by Design.
- Detection, Response & Reporting: Moving from passive governance to active Crisis Handling and automated breach detection.
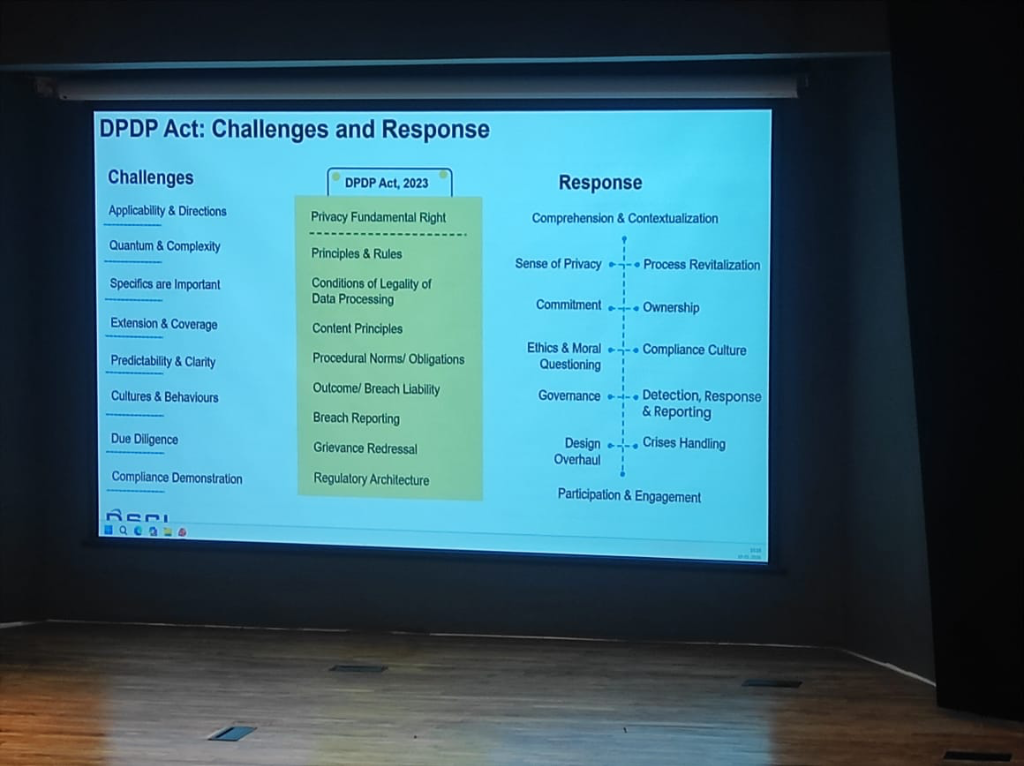 Figure: The strategic roadmap for DPDP Act implementation—transforming institutional culture from passive compliance to active crisis handling.
Figure: The strategic roadmap for DPDP Act implementation—transforming institutional culture from passive compliance to active crisis handling.
Transparency: The Notice & Consent Standard
At the heart of DPDP is a new benchmark for transparency. Institutions must move beyond "fine print" to active disclosure:
-
The Transparency Notice: Hospitals must explicitly inform patients:
- What kind of information is being collected.
- How the information is going to be processed.
- Who all the information is being shared with (Third-party TPAs, Medtech, etc.).
- Why: The specific purpose for which the data is required for service provision.
-
Valid Consent: Consent is no longer a "pre-ticked box." For consent to be valid under DPDP, it must be:
-
Clear, Unambiguous, and Unbundled: It must be a specific, stand-alone permission, not tucked into a general "Terms and Conditions" document.
- Informed Participation: In setups like Teleconsultation, patients must be briefed on the shortcomings and limitations of the platform before their data is processed.
The DPO & The Cultural Shift
A critical component of this legal architecture is the Data Protection Officer (DPO). However, the role faces unique challenges in the Indian context:
- The Query Gap: Currently, DPO-related questions and scrutiny are significantly more mature and frequent outside India. International users and regulators demand more granular data handling details than domestic entities.
- Social Economy & Culture: Privacy governance in India is deeply influenced by our unique social economy and culture. Unlike Western-centric models, Indian privacy must account for a transition from a community-based data sharing culture to a strictly regulated individual rights model.
- From Paper to Practice: Compliance is shifting from "filling forms" to managing real-time data rights. This requires a cultural shift where the DPO is not just a legal signatory but a core part of the hospital's clinical and digital workflow.
Governance & The "CSO Gap"
As Vinayak Godse (CEO, Data Security Council of India - DSCI) emphasizes, the cybersecurity landscape in healthcare is significantly behind other regulated sectors.
- The CSO Absence: Unlike the financial sector, where the Chief Security Officer (CSO) is a mandatory and institutionalized function, most Indian hospitals lack a dedicated leadership role for cybersecurity. Security is often treated as an "IT side-task" rather than a core governance pillar.
- The Banking Comparison: In banking, the RBI has established a rigorous framework that mandates security posture, response protocols, and continuous auditing. Healthcare requires a similar shift from passive protection to active, regulated cybersecurity governance.
- Fragmented Infrastructure Risks: The "fragmented" nature of hospital infrastructure—from legacy on-prem servers to unmanaged medical devices—creates significant data protection gaps and increases vulnerability to ransomware.
- Continuous Posture Improvement: Post-AIIMS, the message is clear: security is not a "fire-and-forget" solution. It requires a continuous improvement of architecture, posture, and response capabilities to stay resilient against evolving threats.
The Evolution of Security Governance
The strategy for protecting medical data has undergone a fundamental shift. As DSCI outlines, the journey moves from passive assurance to active resiliency:
- THEN (Assessment & Assurance): Focus on static Security Controls, Audits, Risk Assessments, and Compliance Verification.
- UNTIL NOW (Real-Time Management): Shift toward Policy Enforcement, Orchestrated and Automated responses, and Predictive situational awareness.
- FROM NOW (Response & Resiliency): The future is Multi-Dimensional Resiliency. This involves Systematized Response and Recovery, Automated Remediation, and Coordinated Communication to limit damage in real-time.
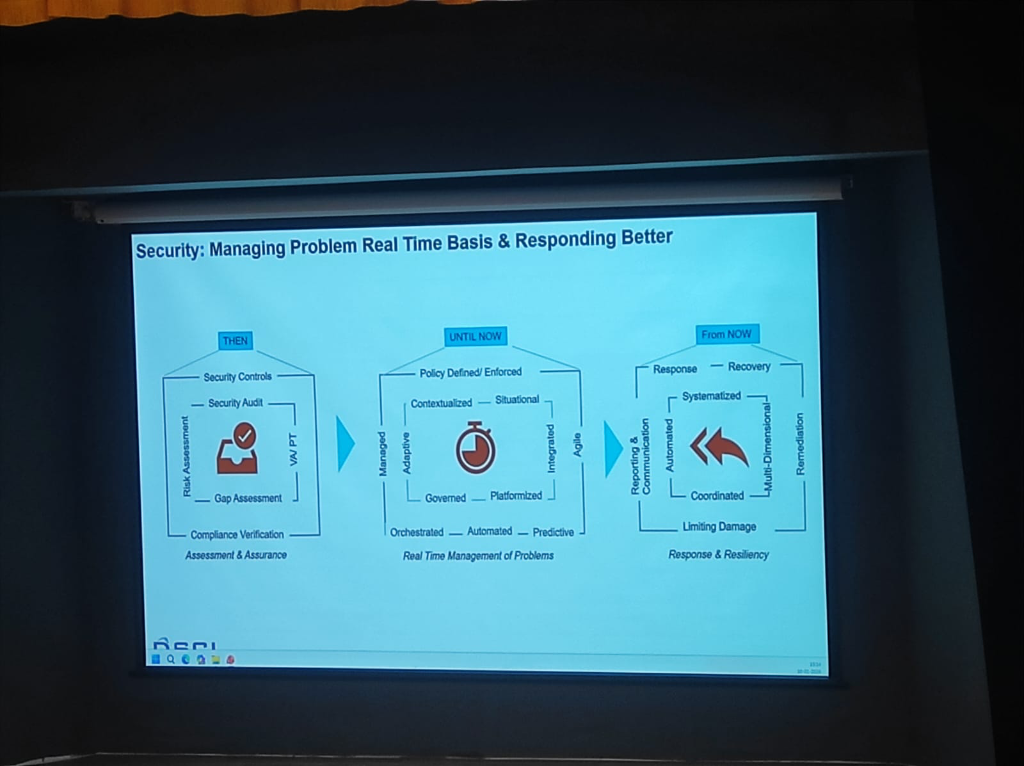 Figure: The paradigm shift in security governance—from audit-based compliance to multi-dimensional clinical resiliency.
Figure: The paradigm shift in security governance—from audit-based compliance to multi-dimensional clinical resiliency.
Threat Vectors in Healthcare
The risk landscape in healthcare has evolved into a multi-layered challenge. As per DSCI’s analysis, these threats can be categorized into three distinct tiers:
- Primary Threats: The foundational risks including Phishing and Social Engineering, Ransomware and Malware, Data Breaches, Credential Stuffing, and Insider Threats (both negligent and malicious).
- Advanced & Complex Threats: Highly targeted attacks such as API Exploits, Supply Chain/Vendor Compromise, Compromised IoMT (Internet of Medical Things), Zero Day Exploits, and Shadow IT/AI.
- Emerging & Uncertain Threats: The next generation of risks featuring AI-Assisted Attacks, Quantum Risk, and Adversarial AI.
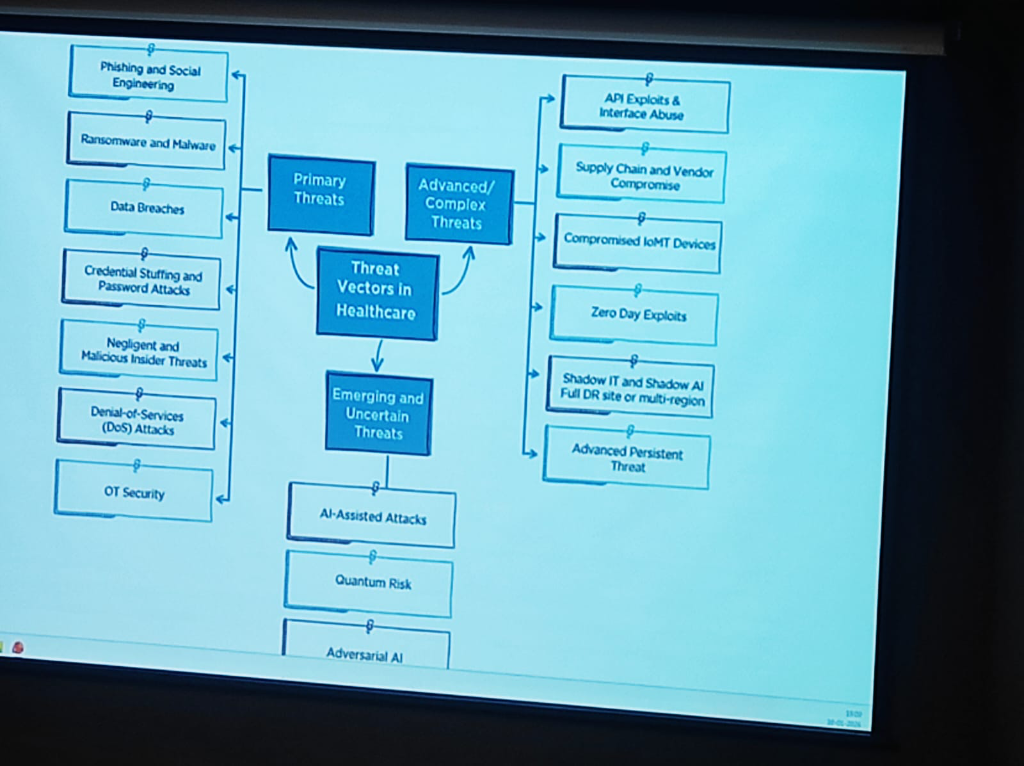 Figure: The evolving landscape of threat vectors in healthcare—from primary breaches to emerging quantum and AI risks.
Figure: The evolving landscape of threat vectors in healthcare—from primary breaches to emerging quantum and AI risks.
Implementing Technical Measures: A 4-Pillar Roadmap
To counter these evolving threats, institutions must move from theoretical security to a rigorous technical implementation roadmap:
- Restrict Access & Multi-Factor Authentication (MFA): Access must be strictly limited to authorized users only. Implementing Multi-Factor Authentication (MFA) across all clinical and administrative applications is non-negotiable for securing the entry points of the HIS.
- Periodical Risk Assessments: Security is dynamic. Hospitals must conduct regular risk assessments to identify technical vulnerabilities, internal loopholes, and the security posture of third-party vendors, service providers, and associates.
- Data Encryption at Scale: Comprehensive Data Encryption must be enforced throughout the information lifecycle—securing data both In Transit (across networks) and At Rest (on storage servers).
- Anonymization & Aggregation: To further mitigate re-identification risks, hospitals should utilize aggregated datasets which significantly decrease the chances of a specific individual being pinpointed from a larger data set.
Ransomware attacks in healthcare are no longer just about encryption; they have become highly advanced technical operations:
- Simultaneous Execution: Modern ransomware executes faster across entire networks, encrypting important files and media simultaneously to prevent manual intervention.
- Botnet & Malware Delivery: Attackers use sophisticated Botnet delivery channels and Command & Control (C2) centers to automate the exfiltration of sensitive patient records.
- The Gen-AI Lowering the Bar: Generative AI has made exploitation easier than ever. It enables attackers to gather footprints, find vulnerabilities, and code malicious payloads with minimal specialized effort.
- A Shared Ecosystem Mandate: This heightened risk requires a unified awareness across the entire ecosystem—Health Providers, Medtech companies, Government agencies, and Insurance providers must all adopt a "Response & Recovery" first mindset.
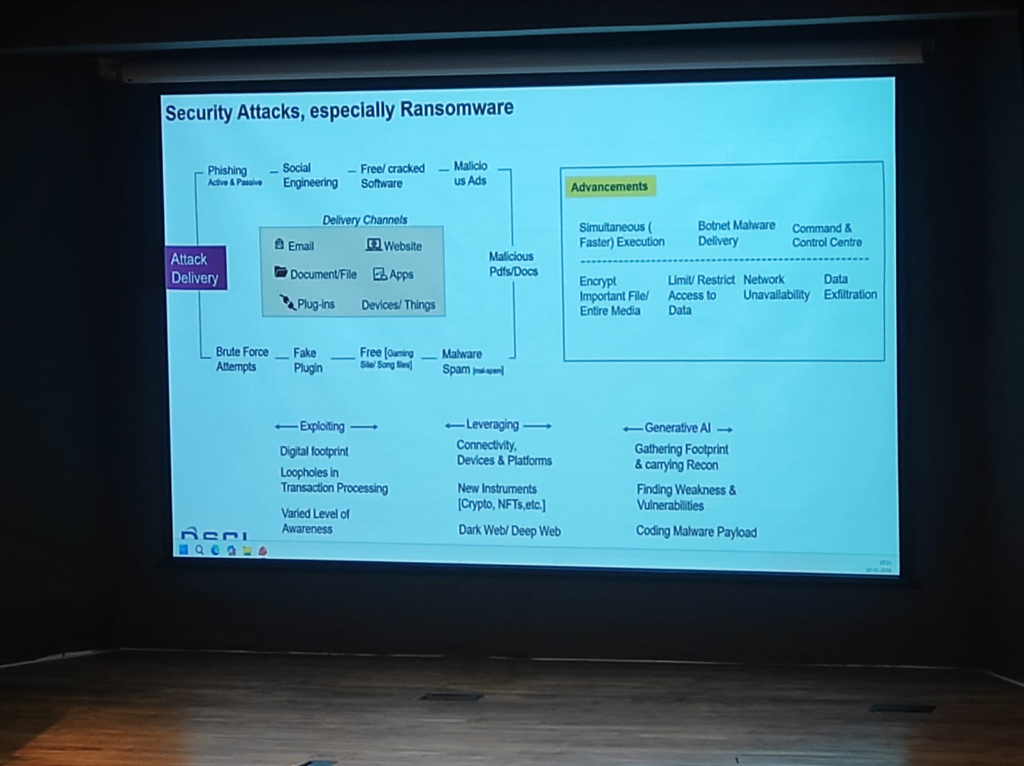 Figure: The technical advancements in ransomware delivery and the role of Generative AI in lowering the barrier for clinical exploitation.
Figure: The technical advancements in ransomware delivery and the role of Generative AI in lowering the barrier for clinical exploitation.
A pervasive but dangerous reality in Indian healthcare is the use of consumer messaging apps like WhatsApp for clinical data exchange:
- Zero Audit Trails: Unlike institutional EMRs, consumer apps provide no standardized logs of who accessed what data and when, making forensic analysis impossible after a breach.
- DPDP Non-Compliance: Sharing personally identifiable health information (PII/PHI) on unmanaged consumer platforms is a direct violation of the DPDP Act. The institution—not the app provider—remains liable for the data leakage.
- The "Shadow Data" Problem: Once a medical report is shared on WhatsApp, it exists in an unmanaged, unencrypted-at-rest state on personal devices, bypassing all institutional security perimeters.
The processing of Insurance Claims and TPA (Third-Party Administrator) interactions remains one of the most neglected areas of data security in Indian healthcare:
- Neglected Security Protocols: While internal clinical systems are increasingly secured, the data sent to insurers often lacks rigorous security SOPs.
- Unsafe Sharing Habits: Sensitive patient claims data is frequently shared through unmanaged, unsecured channels, creating massive exposure risks for both the patient and the hospital.
- The Compliance Gap: Under DPDP, the hospital remains the primary data fiduciary—liable for how the patient's data is handled even when it leaves the premises for insurance processing.
Hospitals often generate and share massive datasets related to Health Surveys and Clinical Trials. These "large-set" exchanges present unique architectural and security challenges:
- Pseudonymization vs. Anonymization: A critical distinction for large-scale data governance:
- Pseudonymization: A technical measure where personal identifiers are replaced by codes. This process is reversible (with a key) and the data is still classified as Personal Data under DPDP.
- Anonymization: A process that irreversibly removes personal identifiers, ensuring the data cannot be traced back to an individual. Anonymized data is generally exempt from certain DPDP processing restrictions.
- The Aggregation Fail: Large datasets are frequently shared in their raw, granular form without proper aggregation, making it easier to re-identify individuals from supposedly "anonymous" lists.
- Mandatory Protocols: For research and survey data to be safe, it must undergo rigorous pseudonymization or anonymization protocols. This ensures that the data is useful for population health analytics without compromising the privacy of the participants.
While the DPDP Act provides certain exemptions for Research, Archiving, and Statistical purposes, these activities must still adhere to rigorous quality standards:
- Lawful Manner: All processing, even for research, must be conducted through legal and ethical frameworks.
- Data Minimization (Necessity): Processing must be limited only to the personal data which is strictly necessary for achieving the research goal.
- Completeness & Accuracy: Researchers are responsible for ensuring the consistency and accuracy of the patient data they handle.
- Reasonable Security Safeguards: Even exempt research data must be protected with modern security measures to prevent leakages.
- Accountability: Every person or institution handling research data remains accountable for the effective observance of these privacy standards.
- Secure Research Sandboxes: Research data should move through managed environments, ensuring that "Person A" cannot be identified through a combination of diverse survey and trial identifiers.
The technical ecosystem of a modern hospital involves dozens of third-party Medtech and software vendors. These represent a major "blind spot" in security governance:
- Supply Chain Vulnerabilities: As seen in global attacks, hackers often target smaller vendors to gain a foothold in larger hospital networks.
- Unmanaged Vendor Access: Allowing vendors "always-on" or unmonitored remote access to clinical systems is a high-risk practice.
- Mandatory Risk Assessments: Institutions must mandate periodic Third-Party Risk Assessments (TPRA) and enforce Least-Privilege Access for all Medtech partners. Managed connectivity (via secure VPCs or ZTNA) is non-negotiable for vendor integrations.
- Contractual Liability: Security is not just technical; it's legal. Vendor contracts must explicitly define breach liability and security standards alignment.
The convergence of rising Quantum complexities, high-velocity data exchanges, and deep cloud dependencies mandates a shift in how hospital architectures are managed:
- Managed Security Architecture: Security is no longer a perimeter firewall; it is a feature of the data flow itself. Architecture must be managed dynamically to counter API exploits, zero-day vulnerabilities, and adversarial AI.
- The Observability Requirement: Hospitals must allocate dedicated budgets for Monitoring and Observability systems. These platforms provide real-time visibility into the "health" of the data ecosystem, detecting anomalies, unauthorized access, and system latencies before they impact patient care.
- Data Flow Integrity: As hospitals become nodes in a national data exchange, observability ensures that every "Scan and Share" or FHIR transaction is secure, audited, and performing at clinical-grade speeds.
As hospitals look toward the future, the role of Artificial Intelligence must be viewed as part of a global paradigm shift. AI is no longer a localized experiment; it is the core engine transforming Autonomous Systems, Manufacturing, Financial Services, E-commerce, Edtech, Space Exploration, Agriculture (Agri), and Cyber Security. Digital Health is the next frontier in this multi-sector revolution, requiring a unique lens for regulatory and security governance:
- Non-FDA Approved LLMs: It is a critical clinical reality that Large Language Models (LLMs) are currently not FDA approved (nor equivalently certified by CDSCO in India) for diagnostic or direct clinical decision-making. They serve as assistive tools, but the clinical liability remains human.
- Diagnostic Accuracy (The Doctor + AI Model): AI is essential for maximizing Diagnostic Accuracy, particularly in screening programs. For instance, Prof. Kshitij Jadhav highlighted a case study on AI-integrated Mammography for breast cancer screening. In India, where there is a high incidence of young breast cancer but no national screening program, a deep learning model was trained to highlight only suspicious lesions and calcifications. By assigning a 1-10 risk score, the AI helps clinicians differentiate between physiological speckles and serious pathologies, significantly improving the "hit rate" compared to systems without AI support.
- Synergy over Replacement: The optimal model remains "Doctor plus AI". The human clinician provides context and nuance, while AI provides the high-velocity pattern recognition required for early detection. The goal is a collaborative synergy where AI acts as a decision-support assistant rather than an autonomous diagnostic "magic wand."
Case Study: AI-Enhanced Triaging Workflow
To visualize why AI is critical for diagnostic accuracy, consider the transformation of the mammography screening workflow (Source: AIDE Lab / KCDH):
graph TD
A[Patient Screening Mammogram] --> B{AI Risk Scoring}
B -- "Low Risk" --> C[Streamlined Review]
B -- "High Risk" --> D[Priority Double Reading]
C --> E[Radiologist Validation]
D --> F[Radiologist 1]
D --> G[Radiologist 2]
F --> H[Consensus]
G --> H
H -- Yes --> I[Final Diagnosis]
H -- No --> J[Senior Radiologist Arbitration]
J --> I
E --> I
style B fill:#e1f5fe,stroke:#01579b,stroke-width:2px
style D fill:#ffebee,stroke:#b71c1c,stroke-width:2px- Standard Workflow (Before AI): Every scan follows a linear path—Radiologist 1 review, followed by Radiologist 2, with the third radiologist acting as an arbitrator only upon disagreement. This is resource-intensive and prone to "screening fatigue."
- AI-Augmented Workflow: The AI system acts as a high-precision triage engine. Scans are assigned a Risk Score (1-10) based on suspicious lesions and calcifications.
- Low-Risk Triaging: Scans with low scores (e.g., 1-5) follow a streamlined validation process.
- High-Risk Prioritization: Scans with high scores (e.g., 6-10) are immediately prioritized for double-reading by specialized radiologists.
- Optimized Recall: By adjusting thresholds, institutions can minimize false positives while ensuring every potential "hit" is captured, maximizing diagnostic accuracy while reducing clinician burden.
| Indicator | Standard Workflow | AI-Augmented Workflow | Impact / Change |
|---|---|---|---|
| Reading Workload | 100% | 66.5% | -33.5% Reduction |
| Cancer Detection Rate | Baseline | Increased | Improved Screening Yield |
| False-Positive Rate | Baseline | Decreased | Reduced Patient Anxiety |
| Turnaround Time | Sequential | Prioritized | Faster High-Risk Results |
Technical Deep Dive: The 4B vs. 1T Parameter Paradox
A critical insight shared during the sessions (Source: Prof. Kshitij Jadhav) centers on the efficiency of AI models in clinical settings.
- The Benchmarking Challenge: Modern LLMs with 1 trillion parameters (often based on massive open-source datasets) reach approximately 90% accuracy on medical benchmarks. However, these models are computationally expensive and difficult to deploy in low-resource clinical environments.
- Ontology-Augmented LLMs: By utilizing Medical Knowledge Graphs and Ontologies (like SNOMED CT) as structured context for LLMs, researchers have achieved a breakthrough in model efficiency.
- Superior Performance at Scale: A specialized 4 billion parameter model, when grounded in a medical knowledge hierarchy, achieves 88-90% accuracy—effectively matching the performance of models hundreds of times its size.
- Low-Resource Deployment: This "Knowledge-First" architecture is essential for India's healthcare landscape, enabling high-precision AI to run on affordable hardware in rural hospitals and clinics where massive GPU clusters are unavailable.
Case Study: Predictive Survival & Triage (Poisoning Control)
Beyond screening, AI is a critical tool for scarce resource allocation. Prof. Kshitij Jadhav discussed a second high-impact use case: Predicting Survival in Rat Poison Ingestion.
graph LR
A[Rat Poison Ingestion] --> B[Integrated Clinical Parameters]
B --> C{AI Prediction Model}
C -- "High Survival Probability" --> D[Supportive Care & Monitoring]
C -- "Critical/Low Survival" --> E[Intensified Triage]
E --> F[Acute Hemodialysis]
E --> G[Liver Exchange Waitlist]
subgraph "Accuracy: 80%"
C
end- The Clinical Challenge: Patients who attempt suicide using rat poison often require intensive supportive therapy, dialysis, or a Liver Exchange.
- Resource Scarcity: India faces a severe shortage of liver donors, making it difficult to decide which patients should be prioritized for transplant vs. supportive therapy.
- The AI Solution: A predictive model was developed to triage these patients. By analyzing clinical parameters, the system achieved 80% accuracy in predicting survival outcomes. This allows clinicians to triage patients effectively, ensuring that high-resource interventions (like liver exchange) are directed where they have the highest probability of life-saving impact.
Case Study: Pan-Cancer Multimodal AI (Histogen)
The frontier of clinical AI lies in Multimodal integration—combining disparate data types for a single patient to enhance Predictive Survival analysis. Prof. Kshitij Jadhav presented the research on Pan-cancer Integrative Histology-Genomic Analysis (Source: Richard J. Chen et al. / AIDE Lab):
graph TD
subgraph "Modality 1: Histopathology"
H["High-Resolution Tissue Images<br/>(WSI)"] --> FE1["Feature Extraction<br/>(CNN/Transformer)"]
end
subgraph "Modality 2: Genomics"
G["Molecular Sequences<br/>(NGS/VCF)"] --> FE2["Genomic Encoding"]
end
FE1 --> F["Multimodal Fusion Layer"]
FE2 --> F
F --> P["Predictive Neural Network"]
P --> Out["<b>Predictive Foresight</b><br/>Distant Metastasis Prediction"]
subgraph "Pan-Cancer Scope: Multiple Malignancies"
Out
end
style F fill:#fff9c4,stroke:#fbc02d,stroke-width:2px
style Out fill:#e8f5e9,stroke:#2e7d32,stroke-width:2pxTo understand the complexity of this model, we must define the technical lexicon of modern oncology AI: - Pan-cancer: Refers to the analysis of multiple different types of cancers simultaneously, identifying common survival patterns across diverse malignancies. - Multimodal Data: The integration of more than one data modality—in this case, combining High-Resolution Histopathology Images (tissue structure) with Genomics Data (molecular sequences). - Multimodal Neural Network: A sophisticated deep learning architecture specifically designed to ingest and process multiple data types simultaneously, fusing their insights into a single clinical output. - Predictive Foresight: By leveraging this multimodal fusion, the model predicts the probability of Distant Metastasis across various cancer types, providing clinicians with a predictive window that single-modality systems cannot achieve.
Prof. Kshitij Jadhav further detailed the broader shifts in this space: - The Shift to Open Source: The world of clinical AI is moving beyond classical localized CNNs. High-performance, Open Source Multimodal Models are emerging, such as Google’s Med-Gemma—a vision-language model that can process both clinical images and text instructions simultaneously. - The Integration Benefit: A critical finding in multimodal research is that while analyzing Genomics or Histopathology in isolation may not show statistically significant prognostic differences, their Fusion (Integration) yields results that are highly significant. This mirrors how doctors actually function—never relying on a single test, but integrating clinical notes, images, and labs to reach a decision. - Path to Personalized Medicine (The 'Holy Grail'): AI is bridging the gap toward the long-promised goal of Personalized Medicine. A key project at Tata Memorial Hospital (TMH)—conducted in Multinational Collaboration with researchers in France and Russia—focuses on Hodgkin’s Lymphoma. The goal is to solve a critical clinical challenge: the administration of high-dosage cytotoxic chemotherapy without a definitive prediction of individual response. - Beyond Binary Diagnosis: While identifying Reed-Sternberg cells confirms a diagnosis of Hodgkin’s vs. Non-Hodgkin’s, researchers are now looking deeper into Whole Slide Images (WSI). - Cell-by-Cell Precision: By annotating slides cell-by-cell—identifying Lymphocytes, Neutrophils, Eosinophils, and Basophils—clinicians have fine-tuned open-source models to achieve 80-85% accuracy in cell identification. - Informed Therapy Selection: This precision allows clinicians to map the Tumor Micro-environment, enabling the prediction of Therapy Response before treatment even begins. This is the "Holy Grail" of oncology—avoiding unnecessary toxicity and directing patients toward the most effective line of therapy from day one.
Decoding the Blueprint: The Role of Genomics & Epigenomics
A foundational pillar of research at KCDH involves understanding human diseases at their most basic level: the DNA, RNA, and the Epigenome.
 Figure: The DNA Blueprint—Adenine (A), Thymine (T), Cytosine (C), and Guanine (G).
Figure: The DNA Blueprint—Adenine (A), Thymine (T), Cytosine (C), and Guanine (G).
- The Foundation of Personalized Medicine: Personalized medicine is not just about the "average" patient; it is about tailoring treatment to the individual's unique biological landscape. This approach depends heavily on the dual understanding of the Genome (the DNA sequence itself) and the Epigenome (the chemical modifications that control how genes are turned on or off).
- The Molecular Signature: Every disease leaves a signature at the molecular level. By studying the ATCG blueprint alongside epigenetic markers, researchers can identify the exact changes and regulatory shifts that drive specific human diseases.
- From Tangential to Central: While often seen as a specialized field, genomics and epigenomics are increasingly central to digital health. The ability to process and analyze these massive datasets allows for a level of Diagnostic and Therapeutic Precision that was previously impossible.
- Digital Health Integration: At KCDH, the focus is on bridging the gap between molecular research and clinical practice. Integrating these genomic and epigenetic "blueprints" into digital health platforms ensures that the patient's individual biological reality is the primary driver of their longitudinal record.
Single-Cell Resolution: The Future of Precision Oncology
The frontier of genomic research at KCDH has moved beyond bulk tissue analysis to Single-Cell RNA Sequencing (scRNA-seq). This technology offers an unprecedented resolution into the cellular composition of tumors, allowing researchers to characterize disease at an individual cell level.
- The Methodology: Cellular Barcoding:
- Dissociation: Tissue (e.g., from the liver or brain) is dissociated into individual cells that are physically separated.
- Unique Identity: Each cell is assigned a unique barcode sequence. This barcode is attached to every RNA molecule extracted from that specific cell, ensuring that even after sequencing, the "molecular identity" of the cell is preserved.
- mRNA Quantification (Poly-A Sequencing): The system captures mRNA molecules (identifiable by their poly-A tails), converts them to cDNA, and sequences them via high-throughput sequencers.
- The "Abundance of Differences" Principle:
- Most physiological issues and disease progressions arise from an abundance of specific proteins or protein-producing sequences.
- By comparing normal vs. cancerous samples, clinicians can quantify exactly how much mRNA each cell possesses, identifying the "abundance of differences" (transcriptomic shifts) that drive disease.
- Precision Targeting: Even within a single organ, cancer may only affect specific cell types. scRNA-seq allows researchers to pinpoint these exact cells among the trillions (36+ trillion) in the human body, avoiding the noise of "bulk" analysis.
- Viral Pathogen Detection: Using advanced algorithms, researchers can now extract Viral Pathogen data (e.g., HPV 16, 18, 54) from human-derived RNA sequences, even when the original assay wasn't designed for it. Recent studies identified HPV 16 expression exclusively within specific clusters of infected cells.
- Reproducible Biomarkers: Because biological data is inherently noisy, KCDH develops advanced statistical models to denoise the data and transition from "one-off" observations to reproducible, clinical-grade biomarkers.
Case Study: Metabolic Associated Fatty Liver Disease (MAFLD)
Beyond oncology and acute poisoning, KCDH is addressing one of India's most widespread yet silent health crises: Non-Alcoholic Fatty Liver Disease (NAFLD), increasingly referred to as Metabolic Associated Fatty Liver Disease (MAFLD).
- The Silent Epidemic: An estimated 1 in 3 individuals in India suffers from a fatty liver. Most cases remain undiagnosed because patients are often asymptomatic until the disease is advanced.
- The Diagnostic Gap: Current gold standards for diagnosis—Ultrasound and Fibroscan—are often reserved for symptomatic patients, leaving millions of early-stage cases undetected.
- The AI Goal: "Single-Drop" Diagnostics: The ultimate objective is to develop a diagnostic tool as simple as a glucose or HbA1c test. By identifying robust immune-system biomarkers in the blood that correlate with liver changes, KCDH aims to enable fatty liver detection from a single drop of blood.
- Overcoming Complexity: Immune changes in the liver are notoriously difficult to characterize. Standard methodologies often struggle with the non-reproducibility of biomarkers across different populations. KCDH is leveraging advanced AI algorithms to identify these elusive, reproducible markers, bridging the gap between clinical research and scalable screening.
Federated Learning: Collaboration Without Data Sharing
One of the most significant barriers to clinical AI is the "Data Silo" problem. Prof. Kshitij Jadhav introduced Federated Learning as the definitive solution for privacy-preserving collaboration: - The Dilemma: Multiple hospitals have vast amounts of similar data, but regulatory and ethical barriers prevent them from sharing raw patient records with each other. - The Architecture: In a Federated system, the raw data never leaves the hospital.
graph TD
subgraph "Hospital A (Local)"
DA["Raw Patient Data"] -.-> LA["Local Model A"]
end
subgraph "Hospital B (Local)"
DB["Raw Patient Data"] -.-> LB["Local Model B"]
end
subgraph "Hospital C (Local)"
DC["Raw Patient Data"] -.-> LC["Local Model C"]
end
subgraph "Central Aggregator"
GM["<b>Global Federated Model</b>"]
end
LA -- "Model Parameters Only" --> GM
LB -- "Model Parameters Only" --> GM
LC -- "Model Parameters Only" --> GM
GM -- "Optimized Learnings" --> LA
GM -- "Optimized Learnings" --> LB
GM -- "Optimized Learnings" --> LC-
Case Study: COVID-19 Triage: This approach was scaled for COVID-19 status prediction. By analyzing routine Vitals and Basic Blood Tests across diverse hospital ecosystems, the federated global model achieved significantly higher accuracy than any individual local model. By learning from the "diversity of scenarios" across institutions without ever seeing a single patient's name, Federated Learning proves that privacy is not a barrier to, but a facilitator of, clinical excellence.
-
Balancing AI & Judgment: Clinicians must balance AI-driven decision support with Clinical Judgment and Patient Preferences. AI should be viewed as an "informed second opinion," where the final diagnostic and therapeutic word always rests with the human clinician and the patient's individual autonomy.
- AI Cybersecurity Risks: Integrating public or non-standardized AI models introduces new attack vectors. Secure clinical AI requires private, HIPAA-compliant instances (VPCs) to ensure patient data never leaks into training sets or public domains.
Data Security: At Rest & In Transit
- Data at Rest: Diagnostic reports and medical images must be secured using AES-256 bit Encryption to ensure data remains unreadable if storage media is compromised.
- Data in Transit: Patient data shared with national backbones like ABDM must be protected using TLS 1.3 / SSL to prevent "man-in-the-middle" attacks.
- DMZ (Demilitarized Zones): Acts as a security buffer, allowing external communication (via VPCs) without exposing core clinical databases.
- RBAC (Role-Based Access Control): Ensures that only authorized personnel can access specific pillars of a patient's medical history.
- Compliance & Audit: Regular automated security audits are mandatory to maintain long-term trust in "my hospital data."
On-Premise vs. Cloud-Native: The Strategic Choice
Institutions must decide where their "brain" resides, balancing control with scalability.
| Feature | On-Premise (Legacy Control) | Cloud-Native (Modern SaaS) | Hybrid (The Indian Reality) |
|---|---|---|---|
| Hosting | Local server rooms with strict HVAC/Fire safety. | Hosted on secure data centers (AWS, Azure, Google). | Tiered: Critical Core on-prem; Scale/Analytics on Cloud. |
| Maintenance | Significant—requires on-site hardware engineers. | Lower—handled by the cloud provider. | Balanced: Internal IT + Managed Cloud Services. |
| Scalability | CapEx-intensive; requires buying new hardware. | Elastic; scales up/down based on demand. | Incremental: Buffer local, burst to Cloud for scale. |
| Connectivity | Fast local LAN; works during internet outages. | Dependent on high-availability internet. | Resilient: Core works offline; Syncs when online. |
| Initial Cost | High upfront investment (Hardware + Setup). | Lower entry cost (Pay-as-you-go). | Moderate: Selective hardware + Subscription OpEx. |
HMIS Governance: Indian vs. Overseas Providers
Choosing the right "brain" for the hospital depends on balancing global maturity with local clinical flexibility.
- The Intent Factor: Institutions with limited internal technical staff should prioritize Cloud-Native Indian providers that offer managed compliance.
- Geographic Reality: For hospitals in regions with internet instability, the Hybrid Deployment remains the gold standard to ensure clinical continuity during outages.
- Regulatory Resilience: Ensure your provider is ABDM-certified and provides a roadmap for DPDP Breach Liability management—this is no longer an optional feature.
Navigating the Challenges of Implementation
Successful digital health transformation encounters several critical challenges, each requiring a dedicated strategic solution.
Critical Challenges & Solutions
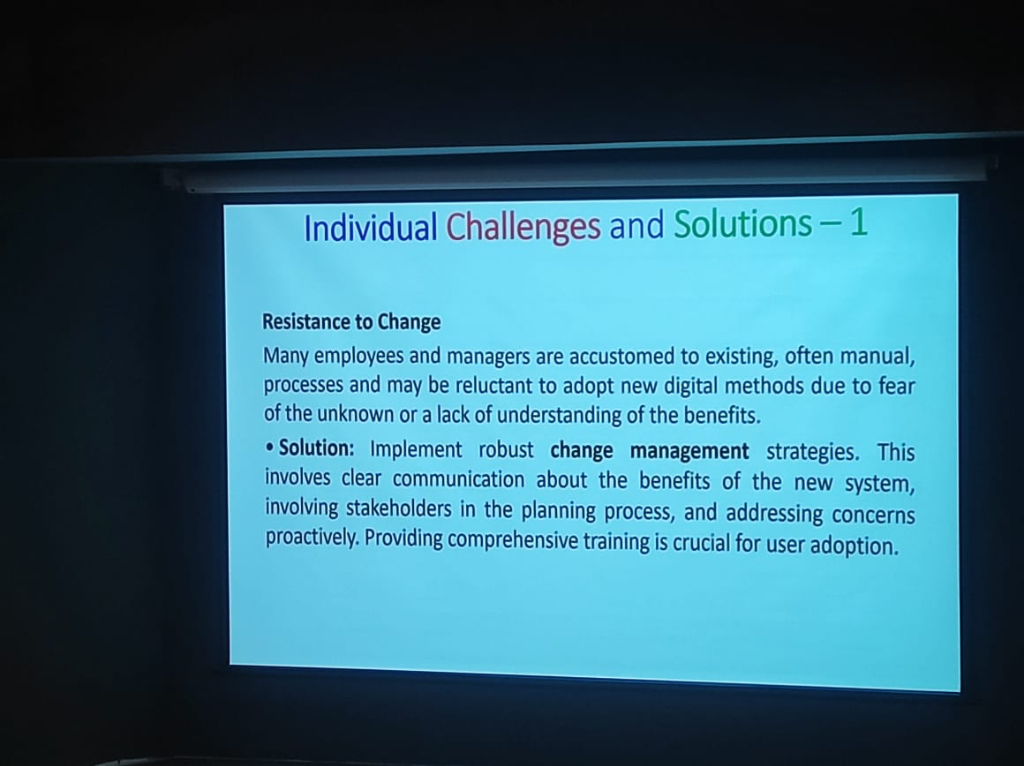 Figure: Managing clinical resistance through robust change management.
Figure: Managing clinical resistance through robust change management.
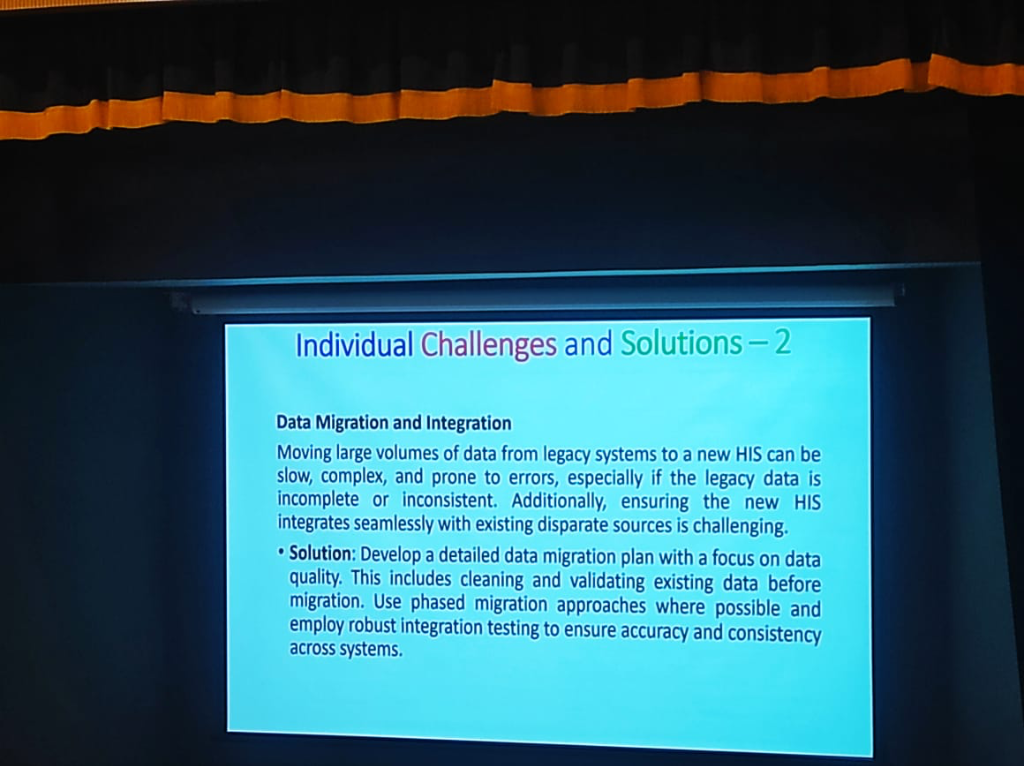 Figure: Ensuring data integrity and operational continuity during migration.
Figure: Ensuring data integrity and operational continuity during migration.
 Figure: Strategic budget planning to prevent scope creep.
Figure: Strategic budget planning to prevent scope creep.
 Figure: Compliance with global standards (ISO, DPDP) for trust.
Figure: Compliance with global standards (ISO, DPDP) for trust.
 Figure: Coordinated project management for complex implementations.
Figure: Coordinated project management for complex implementations.
Key Takeaways: The HABITS Framework
The path to success is paved by building the right institutional HABITS: - Harness Align Build Iterate Transform Sustain.
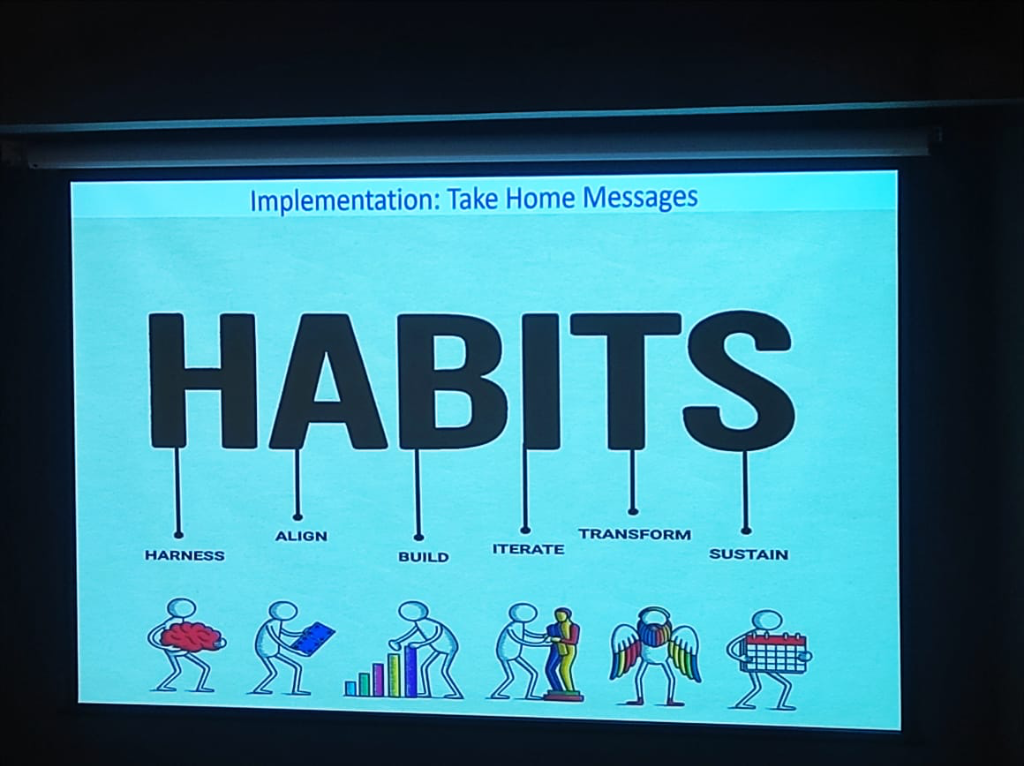
Strategic Impact & Social Responsibility
KCDH’s mission extends beyond technical excellence to social impact and national policy.
Digital Equality & Public Goods
A critical discussion point was the "ROI Gap". Currently, digital transformation is primarily seen in Private Equity (PE) backed hospitals. To achieve Digital Equality and ensure health equity for marginalized populations, we must:
- Acknowledge Non-linear ROI: Digital health does not have a linear Return on Investment. Unlike hardware investments (CT or MRI scanners) where financial recovery is predictable, the ROI for HIS is measured through improved health outcomes and clinical quality—factors that are harder to quantify in short-term financial balance sheets.
- Equitable Access Strategies: Ensuring equitable access requires moving beyond "smartphone-only" models. Strategies must include Assisted Digital Interaction (via ASHAs or ANMs), Multi-lingual Interfaces, and Offline-first Architectures to reach populations with limited technological exposure or internet stability.
- Address the Intent Gap: Identifying and supporting hospitals that show the active intent to digitize, particularly in specialized areas like cancer care planning.
- Support the Koita Foundation: Ensuring funding and resources reach institutions with the highest potential for impact.
- Bridge Infrastructure Gaps: Addressing the critical maintenance and hardware needs in public hospitals to ensure continuous digital functionality.
National & Global Impact: From Care to Research
A major shift is recognizing the duality of medical data:
- Primary Usage: Direct clinical care using systems like EMR, EHR, and CDSS to improve immediate patient outcomes.
- Secondary Usage: Leveraging the same data for National Shared EHRs, clinical research, population health, and statistical analysis.
- Legacy Migration: Large institutions like Tata Memorial Hospital (TMH) face the immense challenge of migrating legacy EMRs (some with 50+ modules) into modern, AI-integrated systems.
- ABDM Integration: Aligning with the Ayushman Bharat Digital Mission to create India's health infrastructure backbone, leveraging FHIR to ensure that every clinical data point is discoverable and interoperable.
The Infrastructure Advantage: India’s Digital Readiness
As highlighted by Prof. Kshitij Jadhav, India is no longer just "digitizing" but is building a robust technological foundation for AI-native healthcare: - Queryable Data vs. Scanned PDFs: A major shift is occurring in top health chains like Max Healthcare and Kokilaben Dhirubhai Ambani Hospital, where clinical data is no longer stored as static scanned PDFs, but as high-quality, Queryable Digital Data. This enables institutional research and real-time AI inference at scale. - The GPU Backbone: India has invested substantially in hardware infrastructure, with a public-private partnership now providing over 30,000 GPUs dedicated to developing sovereign AI solutions. This massive compute capacity allows for the localized training of clinical models that account for Indian physiological and demographic diversity. - The Skills Transfer Principle: AI expertise in India is highly transferable. The advanced engineering talent currently transforming sections like Financial Services, E-commerce, Agriculture (Agri), and Cyber Security is now applying the same rigorous Spark Analysis and deep learning techniques to the clinical space. The same "Skills Stack" that scales a global e-commerce platform is now being leveraged to scale patient-centered digital health.
Demonstrating the Ecosystem in Action
The "Standard Trinity" and NRCeS frameworks aren't just theoretical; they are showcased through powerful live demonstrations that bring these concepts to life for clinicians and engineers alike.
Bridging Research and Practice
-
Synthetic Data Generation: Using the SNOMED CT Implementation Demonstrator, KCDH shows how to generate synthetic patient data based on real-world statistics from the Global Burden of Disease (GBD) Study. This allows for populating EHR systems with realistic test cases reflecting national disease prevalence patterns by age and gender.
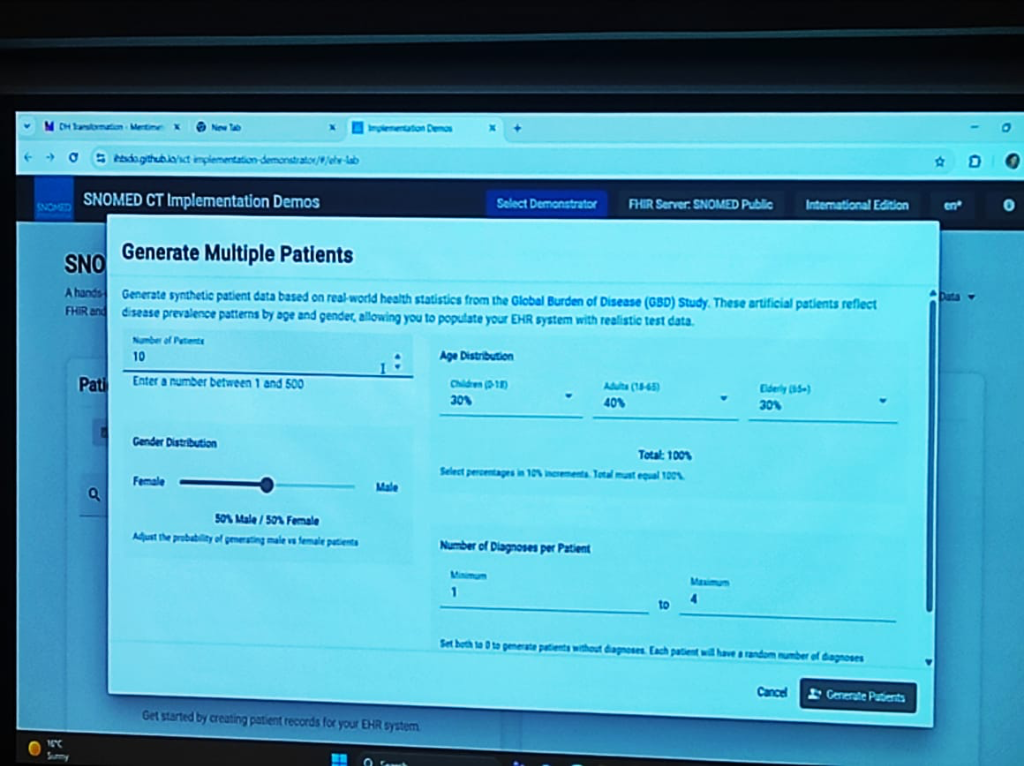
-
AI-Assisted Clinical Forms: The demo showcases FHIR-compliant Clinical Forms—such as Allergy and Intolerance documentation—enhanced with AI-Assisted Entry. This reduces the "key-in" friction for doctors by providing propensity-based models that predict likely clinical outcomes and decision support.
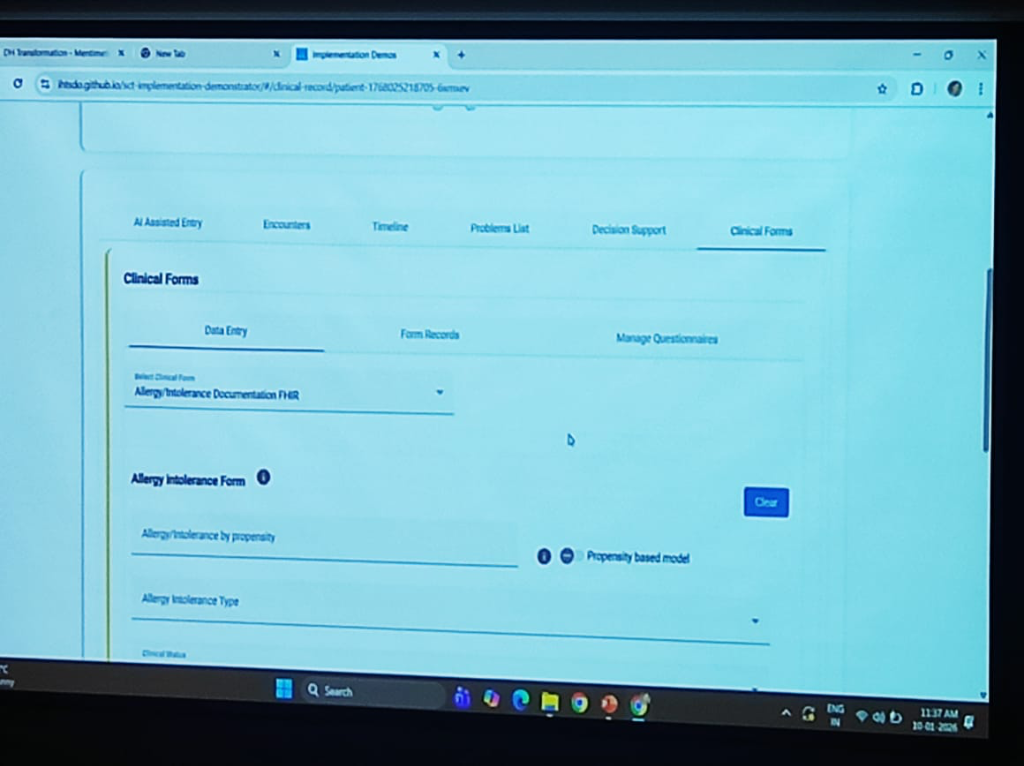
-
Clinical Decision Support (CDS) & Alert Generation: The ecosystem demonstrates real-time CDS Alert Generation. When a clinician adds a problem (e.g., Anaphylaxis) to the Problems List, the system automatically triggers alerts and decision support pathways based on standardized rules (e.g., contraindications or immediate care protocols). This transforms the EHR from a passive repository into an active participant in clinical safety.
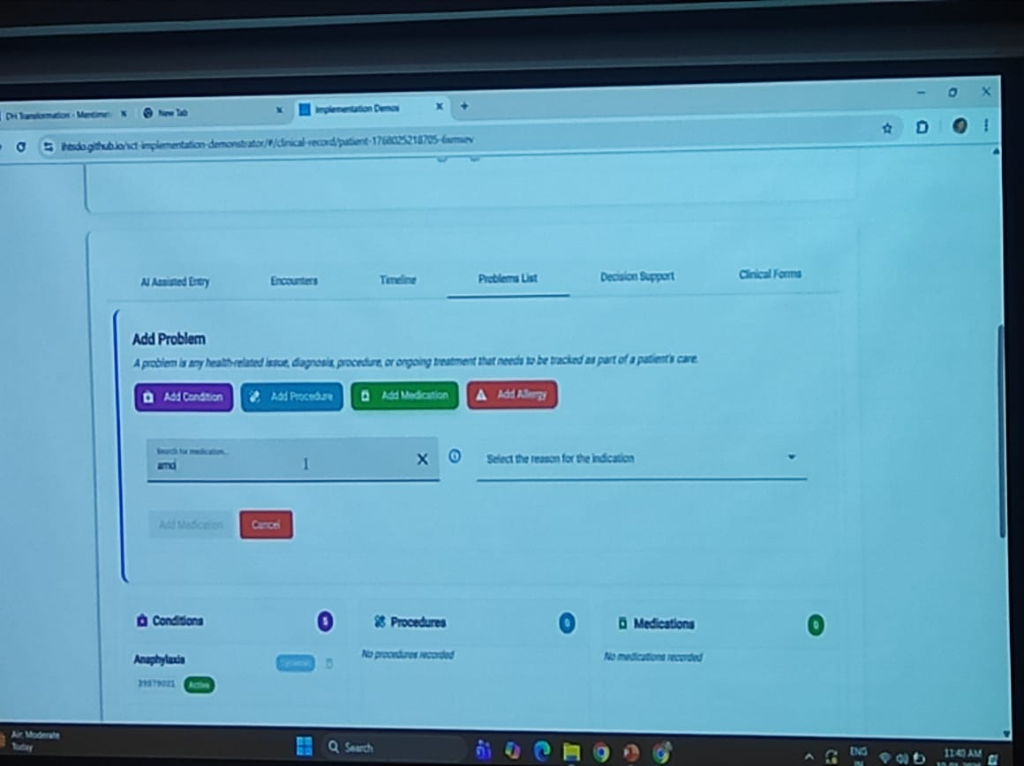
-
Integrated Patient Timeline: Displays a unified problem list, timeline, and decision support—all powered by FHIR and SNOMED CT—providing a template for what a modern, interoperable HIS should look like.
-
Descriptive Population Analysis: The power of standardized coding is best seen at the population level. By using SNOMED CT as the medical coding foundation, the system enables seamless Descriptive Population Analysis. Clinicians and researchers can filter and analyze patient counts by clinical events, age ranges, and gender distributions across the entire repository without any manual data cleaning.
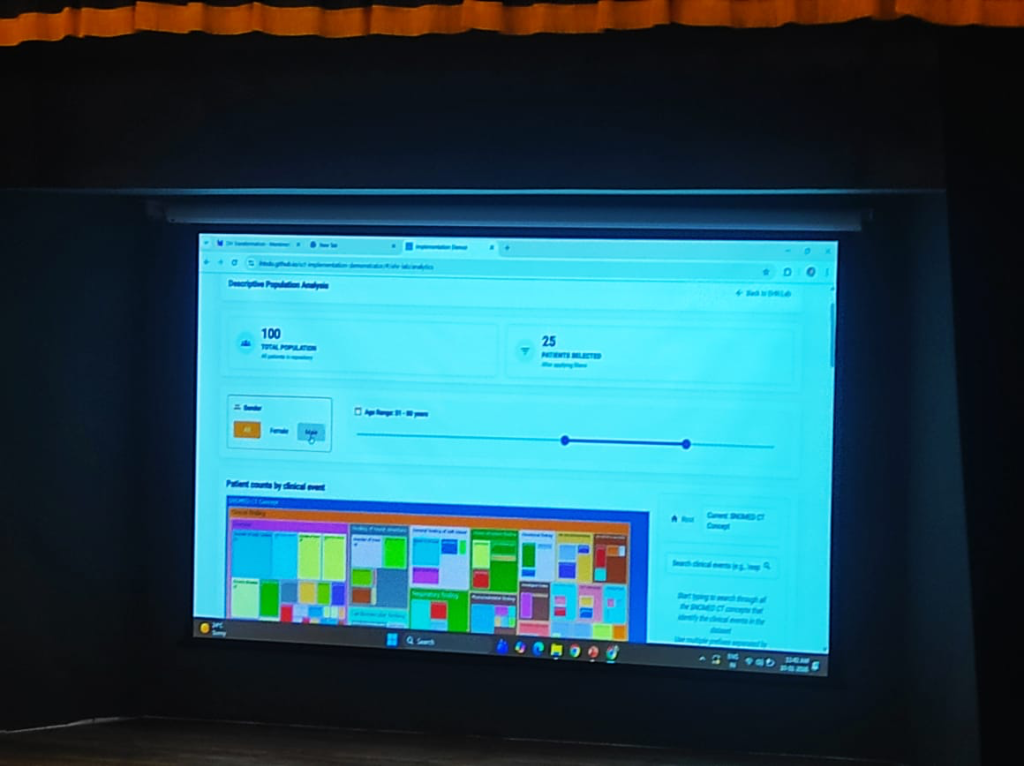
The Way Forward: Building a Connected Ecosystem
The path toward a fully digital healthcare system in India requires a transition from isolated projects to a cohesive national infrastructure.
Strategic Essentials
- Interoperable by Design: Future digital health solutions must be standard-compliant and interoperable from the ground up, rather than attempting to retro-fit integration later.
- User-Driven Solutions: Platforms must be designed with both patients and healthcare providers in mind, ensuring that the technology solves real-world clinical friction instead of adding to it.
- Evidence through Demonstration: Move from theoretical frameworks to demonstrable implementation that proves the value of digital health in real clinical settings.
Infrastructure & Governance
- National & State Level Infrastructure: Establishing robust Discovery Services to identify and catalog healthcare facilities, providers, and services at scale.
- The HIE Backbone: Strengthening the Health Information Exchange (HIE) backbone to facilitate seamless data flow across the country.
- Enforcement & Compliance: Establishing an enforcement authority to address compliance issues and ensure that stakeholders adhere to national health data standards.
Key Strategic Requirements (The Path Ahead)
The transformation of Indian digital health hinges on addressing several core strategic questions. These requirements serve as the benchmark for any institution seeking to achieve true clinical excellence and social impact.
- Rural Literacy: How can doctors in rural areas overcome digital literacy and infrastructure challenges?
- Equitable Access: What strategies can ensure equitable access to digital health tools for marginalized populations?
- AI vs. Judgment: How should clinicians balance AI decision support with clinical judgment and patient preferences?
- Professional Advocacy: What role can professional associations play in capacity building and advocacy for digital health?
- Global Adaptation: How can India’s digital public goods be adapted for global health equity and collaboration?
The Role of Professional Associations
Collective transformation requires more than just individual institutional effort. Professional Associations (such as NABH, DSCI, IMA, and specialty-specific bodies like IAP or API) play a pivotal role in:
- Capacity Building: Organizing cross-institutional training and knowledge-sharing workshops to bridge the digital literacy gap.
- Standard Advocacy: Lobbying for clinical-first standards and ensuring that regulatory mandates (like DPDP) are operationally feasible for front-line doctors.
- Peer Mentorship: Creating networks of "Digital Leaders" who can guide smaller clinics through the complexities of HIS/EMR adoption.
India's Digital Public Goods (DPGs)—specifically the ABDM framework and the NRCeS FHIR profiles—are not just for domestic use. They serve as a Global Blueprint for health equity.
- Adaptability for Global Equity: India's health stack is designed for scale and diversity, making it an ideal template for other developing nations seeking to build interoperable, patient-centric digital health infrastructures.
- Cross-Border Collaboration: By adopting universal standards, India facilitates global research collaboration, allowing for standardized comparative studies on disease burdens and treatment efficacy across diverse populations.
Implementation Roadmap: The Path to Accreditation
Successfully transitioning to a standard-driven institution requires a deliberate, phased approach. Healthcare leaders can follow this 10-step implementation journey:
- Leadership Commitment: Anchoring the transformation in institutional policy and board-level support.
- Digital Masterplan: Defining the long-term architectural and clinical objectives.
- Gap Assessment: Auditing existing systems and infrastructure against national standards.
- Policies & SOPs: Drafting digital clinical protocols and standard operating procedures.
- Software Alignment: Configuring EMR/HIS systems to meet standard specifications.
- Staff Training: Breaking the human barrier through hands-on learning and digital literacy programs.
- Pilot & Scale: Testing the standards in a controlled environment before a full institutional roll-out.
- Internal Audit: Verifying compliance and clinical data integrity internally.
- Accreditation: Moving toward formal recognition under the National Digital Health Standards.
- Continuous Improvement: Establishing an iterative cycle of quality audits and technology updates.
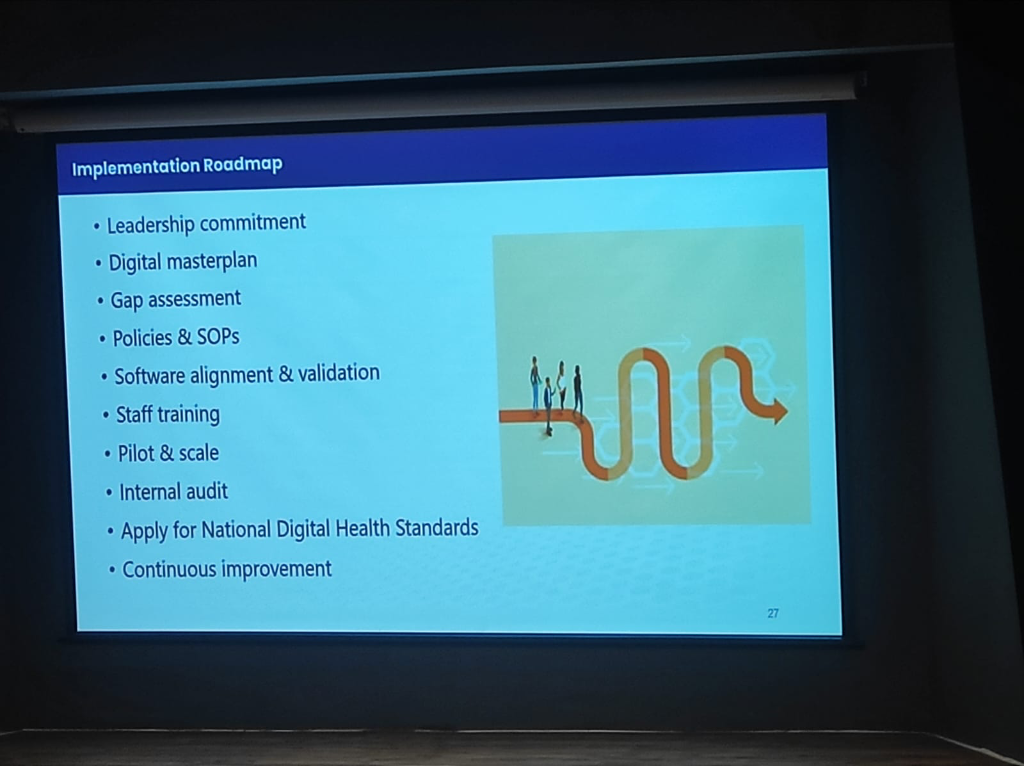 Figure: The 10-step strategic roadmap for hospitals to achieve national digital health accreditation.
Figure: The 10-step strategic roadmap for hospitals to achieve national digital health accreditation.
Conclusion: A Call to Strategic Action
The digital transformation of Indian healthcare is not an IT upgrade; it is a clinical and organizational rebirth. The Koita Centre for Digital Health (KCDH) has demonstrated that the technical blocks—FHIR, SNOMED CT, ABCD—are ready. The question remains: Are the leaders ready?
Breaking the Silos: Quality, Clinical, IT
The most critical takeaway for any healthcare administrator is that these standards are the only tool capable of breaking institutional silos. National Standards (NABH) are inherently superior to proprietary Vendor Standards, which often create "walled gardens" that trap patient data. By adopting national standards, leaders bring together the Quality, Clinical, and IT teams under a single, unified mission: patient safety through data integrity.
The Iterative Approach
We urge healthcare leaders to avoid the "big bang" implementation fallacy. Instead, commit to a progressive, iterative approach.
- Understand the Standards: Move beyond jargon and grasp the operational value of semantic interoperability.
- Motivate Your Teams: Position standards not as a compliance burden, but as the clinical foundation for the next decade.
- Execute and Refine: Start with the "Minimum Data Set" and move incrementally toward total excellence.
As Entheory.AI continues to build the infrastructure for AI-driven clinical workflows, we remain committed to supporting institutions that prioritize these foundational standards. The future of healthcare in India is standardized, secure, and—above all—centered on the patient. Ignoring these mandates is no longer an option; with the Dual Penalty risk of sectoral blacklisting and massive national penalties, the time for digital excellence is now.
Maintained by AlphaPebble Labs
This technical series and its standalone deployment are managed by AlphaPebble Labs.
AlphaPebble Labs specializes in the intersection of Agentic AI, System Resilience, and Clinical Interoperability. We work with leading healthcare institutions and technology providers to implement the standards and architectures discussed in this series—from ABDM-compliant HIEs to advanced AI-augmented clinical workstations.
For more insights into the future of healthcare technology, visit ENTHEORY.AI.